Fatehi M, Hunt C, Ma R, Toyota BD. Persistent Disparities in Survival for Patients with Glioblastoma. World Neurosurg. 2018;120:e511–6.
Rocha Pinheiro SL, Lemos FFB, Marques HS, Silva Luz M, de Oliveira Silva LG. Faria Souza Mendes Dos Santos C, da Costa Evangelista K, Calmon MS, Sande Loureiro M, Freire de Melo F: Immunotherapy in glioblastoma treatment: Current state and future prospects. World J Clin Oncol. 2023;14(4):138–59.
Rominiyi O, Vanderlinden A, Clenton SJ, Bridgewater C, Al-Tamimi Y, Collis SJ. Correction: Tumour treating fields therapy for glioblastoma: current advances and future directions. Br J Cancer. 2021;125(4):623.
van Solinge TS, Nieland L, Chiocca EA, Broekman ML. Advances in local therapy for glioblastoma—taking the fight to the tumour. Nat Rev Neurol. 2022;18(4):221–36.
Efremov L, Abera SF, Bedir A, Vordermark D, Medenwald D. Patterns of glioblastoma treatment and survival over a 16-years period: pooled data from the German Cancer Registries. J Cancer Res Clin Oncol. 2021;147(11):3381–90.
McCutcheon IE, Preul MC. Historical perspective on surgery and survival with glioblastoma: how far have we come? World Neurosurgery. 2021;149:148–68.
Tykocki T, Eltayeb M. Ten-year survival in glioblastoma A systematic review. J Clin Neurosci. 2018;54:7–13.
Hertler C, Felsberg J, Gramatzki D, Le Rhun E, Clarke J, Soffietti R, Wick W, Chinot O, Ducray F, Roth P: Long-term survival with IDH wildtype glioblastoma: first results from the ETERNITY Brain Tumor Funders’ Collaborative Consortium (EORTC 1419). Eur J Cancer 2023.
Cruz Da Silva E, Mercier MC, Etienne-Selloum N, Dontenwill M, Choulier L: A Systematic Review of Glioblastoma-Targeted Therapies in Phases II, III, IV Clinical Trials. Cancers (Basel) 2021, 13(8).
Mandel JJ, Yust-Katz S, Patel AJ, Cachia D, Liu D, Park M, Yuan Y, Kent TA, de Groot JF. Inability of positive phase II clinical trials of investigational treatments to subsequently predict positive phase III clinical trials in glioblastoma. Neuro Oncol. 2018;20(1):113–22.
Poon MTC, Sudlow CLM, Figueroa JD, Brennan PM. Longer-term (>/= 2 years) survival in patients with glioblastoma in population-based studies pre- and post-2005: a systematic review and meta-analysis. Sci Rep. 2020;10(1):11622.
Weeks JC, Catalano PJ, Cronin A, Finkelman MD, Mack JW, Keating NL, Schrag D. Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367(17):1616–25.
Riches JC, Voigt LP. Palliative, Ethics, and End-of-Life Care Issues in the Cancer Patient. Crit Care Clin. 2021;37(1):105–15.
Ostrom QT, Price M, Neff C, Cioffi G, Waite KA, Kruchko C, Barnholtz-Sloan JS: CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2016—2020. Neuro Oncol 2023, 25(Supplement_4):iv1-iv99.
Marenco-Hillembrand L, Wijesekera O, Suarez-Meade P, Mampre D, Jackson C, Peterson J, Trifiletti D, Hammack J, Ortiz K, Lesser E, et al. Trends in glioblastoma: outcomes over time and type of intervention: a systematic evidence based analysis. J Neurooncol. 2020;147(2):297–307.
Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, Ludwin SK, Allgeier A, Fisher B, Belanger K, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009;10(5):459–66.
Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, Hawkins C, Ng HK, Pfister SM, Reifenberger G, et al. The 2021 WHO Classification of Tumors of the Central Nervous System: a summary. Neuro Oncol. 2021;23(8):1231–51.
Brat DJ, Aldape K, Colman H, Figrarella-Branger D, Fuller GN, Giannini C, Holland EC, Jenkins RB, Kleinschmidt-DeMasters B, Komori T, et al. cIMPACT-NOW update 5: recommended grading criteria and terminologies for IDH-mutant astrocytomas. Acta Neuropathol. 2020;139(3):603–8.
Brown NF, Ottaviani D, Tazare J, Gregson J, Kitchen N, Brandner S, Fersht N, Mulholland P. Survival Outcomes and Prognostic Factors in Glioblastoma. Cancers (Basel). 2022;14(13):3161.
Zinn PO, Colen RR, Kasper EM, Burkhardt JK. Extent of resection and radiotherapy in GBM: A 1973 to 2007 surveillance, epidemiology and end results analysis of 21,783 patients. Int J Oncol. 2013;42(3):929–34.
Nieder C, Grosu AL, Astner S, Molls M. Treatment of unresectable glioblastoma multiforme. Anticancer Res. 2005;25(6C):4605–10.
Stupp R, Taillibert S, Kanner A, Read W, Steinberg D, Lhermitte B, Toms S, Idbaih A, Ahluwalia MS, Fink K, et al. Effect of Tumor-Treating Fields Plus Maintenance Temozolomide vs Maintenance Temozolomide Alone on Survival in Patients With Glioblastoma: A Randomized Clinical Trial. JAMA. 2017;318(23):2306–16.
Liau LM, Ashkan K, Brem S, Campian JL, Trusheim JE, Iwamoto FM, Tran DD, Ansstas G, Cobbs CS, Heth JA. Association of autologous tumor lysate-loaded dendritic cell vaccination with extension of survival among patients with newly diagnosed and recurrent glioblastoma: a phase 3 prospective externally controlled cohort trial. JAMA Oncol. 2023;9(1):112–21.
Philip J, Collins A, Brand C, Sundararajan V, Lethborg C, Gold M, Lau R, Moore G, Murphy M. A proposed framework of supportive and palliative care for people with high-grade glioma. Neuro Oncol. 2018;20(3):391–9.
Rivoirard R, Vallard A, Boutet C, Falk AT, Garin C, Adjabi A, Hoarau D, Forest F, Fotso MJ, Rancoule C, et al. A retrospective survey of the last 3 months of life in patients carrying glioblastoma: Clinical treatments and profiles. Mol Clin Oncol. 2018;8(1):115–20.
Network NCC: NCCN guidelines: central nervous system cancers. The NCCN Guidelines 2024, Version 2.2024.
Weller M, van den Bent M, Preusser M, Le Rhun E, Tonn JC, Minniti G, Bendszus M, Balana C, Chinot O, Dirven L, et al. EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat Rev Clin Oncol. 2021;18(3):170–86.
Birzu C, French P, Caccese M, Cerretti G, Idbaih A, Zagonel V, Lombardi G. Recurrent Glioblastoma: From Molecular Landscape to New Treatment Perspectives. Cancers (Basel). 2020;13(1):47.
Seyfried TN, Shelton L, Arismendi-Morillo G, Kalamian M, Elsakka A, Maroon J, Mukherjee P. Provocative Question: Should Ketogenic Metabolic Therapy Become the Standard of Care for Glioblastoma? Neurochem Res. 2019;44(10):2392–404.
Warburg OJS. On the origin of cancer cells. 1956;123(3191):309–14.
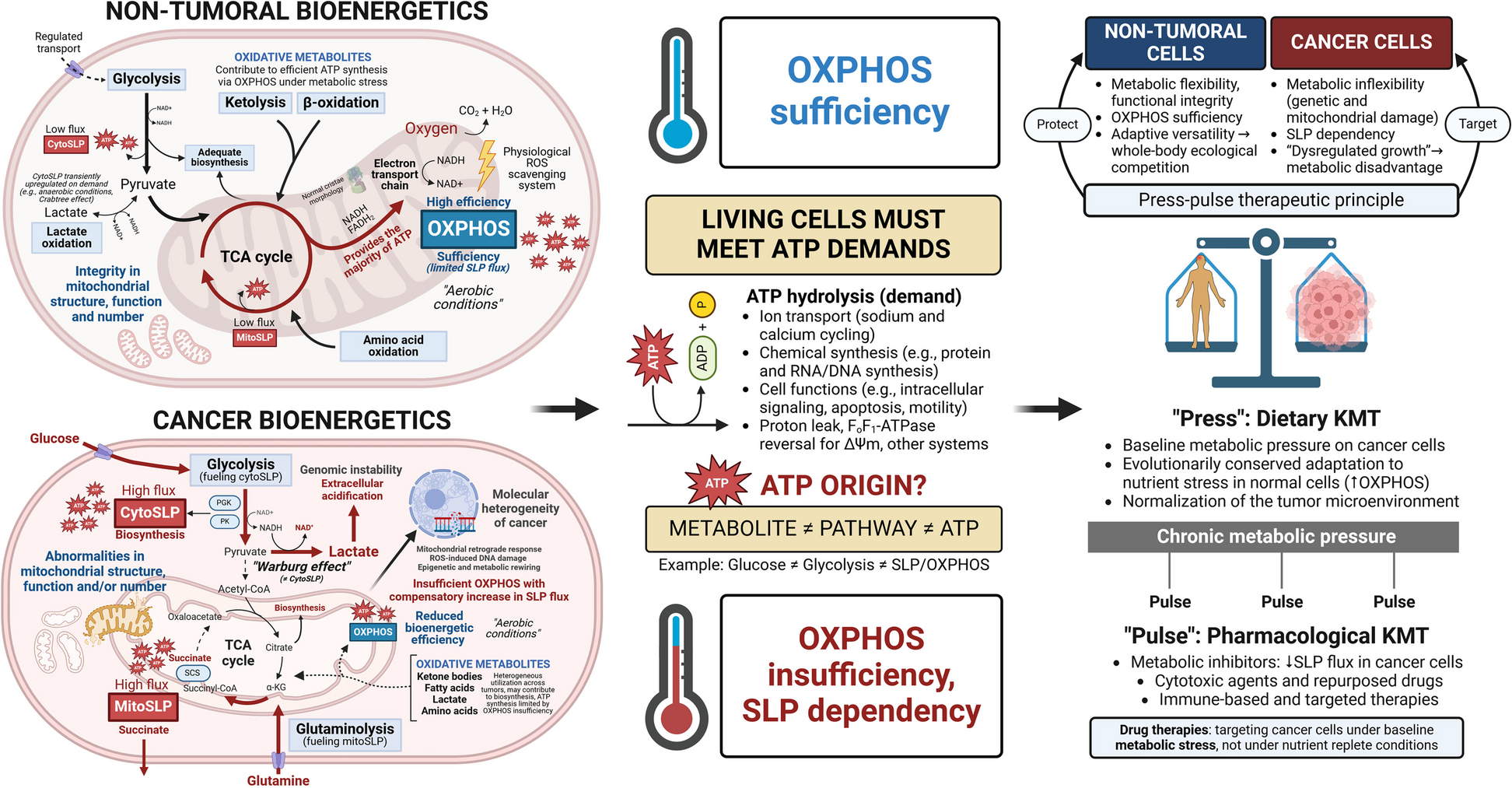
Seyfried TN, Flores RE, Poff AM, D’Agostino DP. Cancer as a metabolic disease: implications for novel therapeutics. Carcinogenesis. 2014;35(3):515–27.
Pfeiffer T, Schuster S, Bonhoeffer S. Cooperation and competition in the evolution of ATP-producing pathways. Science. 2001;292(5516):504–7.
Chinopoulos C, Seyfried TN. Mitochondrial Substrate-Level Phosphorylation as Energy Source for Glioblastoma: Review and Hypothesis. ASN Neuro. 2018;10:1759091418818261.
Ravasz D, Bui D, Nazarian S, Pallag G, Karnok N, Roberts J, Marzullo BP, Tennant DA, Greenwood B, Kitayev A, et al. Residual Complex I activity and amphidirectional Complex II operation support glutamate catabolism through mtSLP in anoxia. Sci Rep. 2024;14(1):1729.
Seyfried TN, Chinopoulos C. Can the mitochondrial metabolic theory explain better the origin and management of cancer than can the somatic mutation theory? Metabolites. 2021;11(9):572.
Altman BJ, Stine ZE, Dang CV. From Krebs to clinic: glutamine metabolism to cancer therapy. Nat Rev Cancer. 2016;16(10):619–34.
Wise DR, DeBerardinis RJ, Mancuso A, Sayed N, Zhang XY, Pfeiffer HK, Nissim I, Daikhin E, Yudkoff M, McMahon SB, et al. Myc regulates a transcriptional program that stimulates mitochondrial glutaminolysis and leads to glutamine addiction. Proc Natl Acad Sci U S A. 2008;105(48):18782–7.
Oizel K, Chauvin C, Oliver L, Gratas C, Geraldo F, Jarry U, Scotet E, Rabe M, Alves-Guerra MC, Teusan R, et al. Efficient Mitochondrial Glutamine Targeting Prevails Over Glioblastoma Metabolic Plasticity. Clin Cancer Res. 2017;23(20):6292–304.
Maraqah HH, Abu-Asab MS, Lee HS, Aboud O. Comparative survey of mitochondrial ultrastructure in IDH1-mutant astrocytoma and IDH1-wildtype glioblastoma (GBM). Ultrastruct Pathol. 2023;47(2):1–6.
Deighton RF, Le Bihan T, Martin SF, Gerth AMJ, McCulloch M, Edgar JM, Kerr LE, Whittle IR, McCulloch J. Interactions among mitochondrial proteins altered in glioblastoma. J Neurooncol. 2014;118(2):247–56.
Arismendi-Morillo G, Castellano-Ramirez A, Seyfried TN. Ultrastructural characterization of the Mitochondria-associated membranes abnormalities in human astrocytomas: Functional and therapeutics implications. Ultrastruct Pathol. 2017;41(3):234–44.
Feichtinger RG, Weis S, Mayr JA, Zimmermann F, Geilberger R, Sperl W, Kofler B. Alterations of oxidative phosphorylation complexes in astrocytomas. Glia. 2014;62(4):514–25.
Kossenkov AV, Milcarek A, Notta F, Jang GH, Wilson JM, Gallinger S, Zhou DC, Ding L, Ghosh JC, Perego M, et al. Mitochondrial fitness and cancer risk. PLoS ONE. 2022;17(10): e0273520.
Srinivasan S, Guha M, Kashina A, Avadhani NG. Mitochondrial dysfunction and mitochondrial dynamics-The cancer connection. Biochim Biophys Acta Bioenerg. 2017;1858(8):602–14.
Ghosh JC, Perego M, Agarwal E, Bertolini I, Wang Y, Goldman AR, Tang HY, Kossenkov AV, Landis CJ, Languino LR, et al. Ghost mitochondria drive metastasis through adaptive GCN2/Akt therapeutic vulnerability. Proc Natl Acad Sci U S A. 2022;119(8): e2115624119.
Yao T, Asayama Y. Animal-cell culture media: History, characteristics, and current issues. Reprod Med Biol. 2017;16(2):99–117.
Pavlova NN, Thompson CB. The Emerging Hallmarks of Cancer Metabolism. Cell Metab. 2016;23(1):27–47.
Eagle H. Amino acid metabolism in mammalian cell cultures. Science. 1959;130(3373):432–7.
Hall A, Meyle KD, Lange MK, Klima M, Sanderhoff M, Dahl C, Abildgaard C, Thorup K, Moghimi SM, Jensen PB, et al. Dysfunctional oxidative phosphorylation makes malignant melanoma cells addicted to glycolysis driven by the (V600E)BRAF oncogene. Oncotarget. 2013;4(4):584–99.
Gouirand V, Gicquel T, Lien EC, Jaune-Pons E, Da Costa Q, Finetti P, Metay E, Duluc C, Mayers JR, Audebert S, et al. Ketogenic HMG-CoA lyase and its product beta-hydroxybutyrate promote pancreatic cancer progression. EMBO J. 2022;41(9): e110466.
Sperry J, Condro MC, Guo L, Braas D, Vanderveer-Harris N, Kim KKO, Pope WB, Divakaruni AS, Lai A, Christofk H et al: Glioblastoma Utilizes Fatty Acids and Ketone Bodies for Growth Allowing Progression during Ketogenic Diet Therapy. iScience 2020, 23(9):101453.
Santiappillai NT, Hakeem-Sanni MF, Ghasemi M, Withy A, Quek L-E, Hoy AJ: Fatty acids are not a significant contributor to the TCA cycle in cancer cell lines: evidence of incomplete fatty acid oxidation. bioRxiv 2024:2024.2003. 2025.586547.
Altea-Manzano P, Cuadros AM, Broadfield LA, Fendt SM. Nutrient metabolism and cancer in the in vivo context: a metabolic game of give and take. EMBO Rep. 2020;21(10): e50635.
Cluntun AA, Lukey MJ, Cerione RA, Locasale JW. Glutamine Metabolism in Cancer: Understanding the Heterogeneity. Trends Cancer. 2017;3(3):169–80.
Faubert B, Li KY, Cai L, Hensley CT, Kim J, Zacharias LG, Yang C, Do QN, Doucette S, Burguete D et al: Lactate Metabolism in Human Lung Tumors. Cell 2017, 171(2):358–371 e359.
Warburg O. On respiratory impairment in cancer cells. Science. 1956;124(3215):269–70.
Weinhouse S. The Warburg hypothesis fifty years later. Zeitschrift fur Krebsforschung und klinische Onkologie. 1976;87(2):115–26.
Bartman CR, Weilandt DR, Shen Y, Lee WD, Han Y, TeSlaa T, Jankowski CSR, Samarah L, Park NR, da Silva-Diz V, et al. Slow TCA flux and ATP production in primary solid tumours but not metastases. Nature. 2023;614(7947):349–57.
Viale A, Pettazzoni P, Lyssiotis CA, Ying H, Sanchez N, Marchesini M, Carugo A, Green T, Seth S, Giuliani V, et al. Oncogene ablation-resistant pancreatic cancer cells depend on mitochondrial function. Nature. 2014;514(7524):628–32.
Ju YS, Alexandrov LB, Gerstung M, Martincorena I, Nik-Zainal S, Ramakrishna M, Davies HR, Papaemmanuil E, Gundem G, Shlien A, et al. Origins and functional consequences of somatic mitochondrial DNA mutations in human cancer. Elife. 2014;3: e02935.
Duraj T, Carrion-Navarro J, Seyfried TN, Garcia-Romero N, Ayuso-Sacido A. Metabolic therapy and bioenergetic analysis: The missing piece of the puzzle. Mol Metab. 2021;54: 101389.
Zhang J, Jia PP, Liu QL, Cong MH, Gao Y, Shi HP, Yu WN, Miao MY. Low ketolytic enzyme levels in tumors predict ketogenic diet responses in cancer cell lines in vitro and in vivo. J Lipid Res. 2018;59(4):625–34.
Maurer GD, Brucker DP, Bahr O, Harter PN, Hattingen E, Walenta S, Mueller-Klieser W, Steinbach JP, Rieger J. Differential utilization of ketone bodies by neurons and glioma cell lines: a rationale for ketogenic diet as experimental glioma therapy. BMC Cancer. 2011;11(1):315.
Skinner R, Trujillo A, Ma X, Beierle EA: Ketone bodies inhibit the viability of human neuroblastoma cells. J Pediatr Surg 2009, 44(1):212–216; discussion 216.
Artzi M, Liberman G, Vaisman N, Bokstein F, Vitinshtein F, Aizenstein O, Ben Bashat D. Changes in cerebral metabolism during ketogenic diet in patients with primary brain tumors: (1)H-MRS study. J Neurooncol. 2017;132(2):267–75.
Voss M, Lorenz NI, Luger AL, Steinbach JP, Rieger J, Ronellenfitsch MW. Rescue of 2-Deoxyglucose Side Effects by Ketogenic Diet. Int J Mol Sci. 2018;19(8):2462.
Mukherjee P, Augur ZM, Li M, Hill C, Greenwood B, Domin MA, Kondakci G, Narain NR, Kiebish MA, Bronson RT, et al. Therapeutic benefit of combining calorie-restricted ketogenic diet and glutamine targeting in late-stage experimental glioblastoma. Commun Biol. 2019;2(1):200.
Hopkins BD, Pauli C, Du X, Wang DG, Li X, Wu D, Amadiume SC, Goncalves MD, Hodakoski C, Lundquist MR. Suppression of insulin feedback enhances the efficacy of PI3K inhibitors. Nature. 2018;560(7719):499–503.
Hajihassani O, Zarei M, Roichman A, Loftus A, Boutros CS, Hue J, Naji P, Boyer J, Tahan S, Gallagher P et al: A Ketogenic Diet Sensitizes Pancreatic Cancer to Inhibition of Glutamine Metabolism. bioRxiv 2024:2024.2007. 2019.604377.
Stine ZE, Schug ZT, Salvino JM, Dang CV. Targeting cancer metabolism in the era of precision oncology. Nat Rev Drug Discov. 2022;21(2):141–62.
Yang WH, Qiu Y, Stamatatos O, Janowitz T, Lukey MJ. Enhancing the Efficacy of Glutamine Metabolism Inhibitors in Cancer Therapy. Trends Cancer. 2021;7(8):790–804.
Kawai T, Brender JR, Lee JA, Kramp T, Kishimoto S, Krishna MC, Tofilon P, Camphausen KA. Detection of metabolic change in glioblastoma cells after radiotherapy using hyperpolarized 13C-MRI. NMR Biomed. 2021;34(7): e4514.
Wibom C, Surowiec I, Moren L, Bergstrom P, Johansson M, Antti H, Bergenheim AT. Metabolomic patterns in glioblastoma and changes during radiotherapy: a clinical microdialysis study. J Proteome Res. 2010;9(6):2909–19.
Bergsneider M, Hovda DA, Shalmon E, Kelly DF, Vespa PM, Martin NA, Phelps ME, McArthur DL, Caron MJ, Kraus JF, et al. Cerebral hyperglycolysis following severe traumatic brain injury in humans: a positron emission tomography study. J Neurosurg. 1997;86(2):241–51.
Seyfried TN, Shelton LM, Mukherjee P. Does the existing standard of care increase glioblastoma energy metabolism? Lancet Oncol. 2010;11(9):811–3.
Oliva CR, Nozell SE, Diers A, McClugage SG 3rd, Sarkaria JN, Markert JM, Darley-Usmar VM, Bailey SM, Gillespie GY, Landar A, et al. Acquisition of temozolomide chemoresistance in gliomas leads to remodeling of mitochondrial electron transport chain. J Biol Chem. 2010;285(51):39759–67.
Johnson BE, Mazor T, Hong C, Barnes M, Aihara K, McLean CY, Fouse SD, Yamamoto S, Ueda H, Tatsuno K, et al. Mutational analysis reveals the origin and therapy-driven evolution of recurrent glioma. Science. 2014;343(6167):189–93.
Winter SF, Loebel F, Loeffler J, Batchelor TT, Martinez-Lage M, Vajkoczy P, Dietrich J. Treatment-induced brain tissue necrosis: a clinical challenge in neuro-oncology. Neuro Oncol. 2019;21(9):1118–30.
Wen PY, Weller M, Lee EQ, Alexander BM, Barnholtz-Sloan JS, Barthel FP, Batchelor TT, Bindra RS, Chang SM, Chiocca EA, et al. Glioblastoma in adults: a Society for Neuro-Oncology (SNO) and European Society of Neuro-Oncology (EANO) consensus review on current management and future directions. Neuro Oncol. 2020;22(8):1073–113.
Pitter KL, Tamagno I, Alikhanyan K, Hosni-Ahmed A, Pattwell SS, Donnola S, Dai C, Ozawa T, Chang M, Chan TA, et al. Corticosteroids compromise survival in glioblastoma. Brain. 2016;139(Pt 5):1458–71.
Klement RJ, Champ CE. Corticosteroids compromise survival in glioblastoma in part through their elevation of blood glucose levels. Brain. 2017;140(3): e16.
Wong ET, Lok E, Gautam S, Swanson KD. Dexamethasone exerts profound immunologic interference on treatment efficacy for recurrent glioblastoma. Br J Cancer. 2015;113(2):232–41.
Decker M, Sacks P, Abbatematteo J, De Leo E, Brennan M, Rahman M. The effects of hyperglycemia on outcomes in surgical high-grade glioma patients. Clin Neurol Neurosurg. 2019;179:9–13.
McGirt MJ, Chaichana KL, Gathinji M, Attenello F, Than K, Jimenez Ruiz A, Olivi A, Quinones-Hinojosa A: Persistent outpatient hyperglycemia is independently associated with decreased survival after primary resection of malignant brain astrocytomas. Neurosurgery 2008, 63(2):286–291; discussion 291.
Derr RL, Ye X, Islas MU, Desideri S, Saudek CD, Grossman SA. Association between hyperglycemia and survival in patients with newly diagnosed glioblastoma. J Clin Oncol. 2009;27(7):1082–6.
Mayer A, Vaupel P, Struss HG, Giese A, Stockinger M, Schmidberger H. Strong adverse prognostic impact of hyperglycemic episodes during adjuvant chemoradiotherapy of glioblastoma multiforme. Strahlenther Onkol. 2014;190(10):933–8.
Tieu MT, Lovblom LE, McNamara MG, Mason W, Laperriere N, Millar BA, Menard C, Kiehl TR, Perkins BA, Chung C. Impact of glycemia on survival of glioblastoma patients treated with radiation and temozolomide. J Neurooncol. 2015;124(1):119–26.
Swildens KX, Sillevis Smitt PAE, van den Bent MJ, French PJ, Geurts M: The effect of dexamethasone on the microenvironment and efficacy of checkpoint inhibitors in glioblastoma: a systematic review. Neurooncol Adv 2022, 4(1):vdac087.
Caramanna I, de Kort JM, Brandes AA, Taal W, Platten M, Idbaih A, Frenel JS, Wick W, Preetha CJ, Bendszus M, et al. Corticosteroids use and neurocognitive functioning in patients with recurrent glioblastoma: Evidence from European Organization for Research and Treatment of Cancer (EORTC) trial 26101. Neurooncol Pract. 2022;9(4):310–6.
Mantilla EC Jr, Abramowitz J, Dan TU, Pan E. Prolonged Steroid Dependence in Adult Patients With Glioma. Anticancer Res. 2020;40(4):2059–64.
Petrelli F, De Stefani A, Ghidini A, Bruschieri L, Riboldi V, Dottorini L, Iaculli A, Zaniboni A, Trevisan F. Steroids use and survival in patients with glioblastoma multiforme: a pooled analysis. J Neurol. 2021;268(2):440–7.
Paez-Ribes M, Allen E, Hudock J, Takeda T, Okuyama H, Vinals F, Inoue M, Bergers G, Hanahan D, Casanovas O. Antiangiogenic therapy elicits malignant progression of tumors to increased local invasion and distant metastasis. Cancer Cell. 2009;15(3):220–31.
de Groot JF, Fuller G, Kumar AJ, Piao Y, Eterovic K, Ji Y, Conrad CA. Tumor invasion after treatment of glioblastoma with bevacizumab: radiographic and pathologic correlation in humans and mice. Neuro Oncol. 2010;12(3):233–42.
Thompson EM, Frenkel EP, Neuwelt EA. The paradoxical effect of bevacizumab in the therapy of malignant gliomas. Neurology. 2011;76(1):87–93.
Van Kleffens T, van Baarsen B, van Leeuwen E. The medical practice of patient autonomy and cancer treatment refusals: a patients’ and physicians’ perspective. Social science medicine. 2004;58(11):2325–36.
Drolet BC, White CL. Selective paternalism. Virtual Mentor. 2012;14(7):582–8.
Peppercorn J. Ethics of ongoing cancer care for patients making risky decisions. J Oncol Pract. 2012;8(5):e111–113.
Tenner L, Hlubocky FJ, Blanke CD, LeBlanc TW, Marron JM, McGinnis MM, Spence RA, Taylor LP. Let’s talk about those herbs you are taking: ethical considerations for communication with patients with cancer about complementary and alternative medicine. Journal of oncology practice. 2019;15(1):44–9.
Winter SF, Loebel F, Dietrich J. Role of ketogenic metabolic therapy in malignant glioma: A systematic review. Crit Rev Oncol Hematol. 2017;112:41–58.
Woolf EC, Syed N, Scheck AC. Tumor Metabolism, the Ketogenic Diet and beta-Hydroxybutyrate: Novel Approaches to Adjuvant Brain Tumor Therapy. Front Mol Neurosci. 2016;9:122.
Schwartz KA, Noel M, Nikolai M, Olson LK, Hord NG, Zakem M, Clark J, Elnabtity M, Figueroa B, Chang HT. Long Term Survivals in Aggressive Primary Brain Malignancies Treated With an Adjuvant Ketogenic Diet. Front Nutr. 2022;9: 770796.
Hagihara K, Kajimoto K, Osaga S, Nagai N, Shimosegawa E, Nakata H, Saito H, Nakano M, Takeuchi M, Kanki H et al: Promising Effect of a New Ketogenic Diet Regimen in Patients with Advanced Cancer. Nutrients 2020, 12(5).
Iyikesici MS. Feasibility study of metabolically supported chemotherapy with weekly carboplatin/paclitaxel combined with ketogenic diet, hyperthermia and hyperbaric oxygen therapy in metastatic non-small cell lung cancer. Int J Hyperthermia. 2019;36(1):446–55.
Iyikesici MS, Slocum AK, Slocum A, Berkarda FB, Kalamian M, Seyfried TN. Efficacy of Metabolically Supported Chemotherapy Combined with Ketogenic Diet, Hyperthermia, and Hyperbaric Oxygen Therapy for Stage IV Triple-Negative Breast Cancer. Cureus. 2017;9(7): e1445.
Khodabakhshi A, Akbari ME, Mirzaei HR, Seyfried TN, Kalamian M, Davoodi SH. Effects of Ketogenic metabolic therapy on patients with breast cancer: A randomized controlled clinical trial. Clin Nutr. 2021;40(3):751–8.
Maroon J, Bost J, Amos A, Zuccoli G. Restricted calorie ketogenic diet for the treatment of glioblastoma multiforme. J Child Neurol. 2013;28(8):1002–8.
Zuccoli G, Marcello N, Pisanello A, Servadei F, Vaccaro S, Mukherjee P, Seyfried TN. Metabolic management of glioblastoma multiforme using standard therapy together with a restricted ketogenic diet: Case Report. Nutr Metab (Lond). 2010;7(1):33.
Panhans CM, Gresham G, Amaral LJ, Hu J. Exploring the Feasibility and Effects of a Ketogenic Diet in Patients With CNS Malignancies: A Retrospective Case Series. Front Neurosci. 2020;14:390.
Elsakka AMA, Bary MA, Abdelzaher E, Elnaggar M, Kalamian M, Mukherjee P, Seyfried TN. Management of Glioblastoma Multiforme in a Patient Treated With Ketogenic Metabolic Therapy and Modified Standard of Care: A 24-Month Follow-Up. Front Nutr. 2018;5:20.
Martuscello RT, Vedam-Mai V, McCarthy DJ, Schmoll ME, Jundi MA, Louviere CD, Griffith BG, Skinner CL, Suslov O, Deleyrolle LP, et al. A Supplemented High-Fat Low-Carbohydrate Diet for the Treatment of Glioblastoma. Clin Cancer Res. 2016;22(10):2482–95.
Rieger J, Bahr O, Maurer GD, Hattingen E, Franz K, Brucker D, Walenta S, Kammerer U, Coy JF, Weller M, et al. ERGO: a pilot study of ketogenic diet in recurrent glioblastoma. Int J Oncol. 2014;44(6):1843–52.
Klein P, Tyrlikova I, Zuccoli G, Tyrlik A, Maroon JC. Treatment of glioblastoma multiforme with “classic” 4:1 ketogenic diet total meal replacement. Cancer Metab. 2020;8(1):24.
Tan-Shalaby JL, Carrick J, Edinger K, Genovese D, Liman AD, Passero VA, Shah RB. Modified Atkins diet in advanced malignancies-final results of a safety and feasibility trial within the Veterans Affairs Pittsburgh Healthcare System. Nutrition metabolism. 2016;13(1):1–12.
Buga A, Harper DG, Sapper TN, Hyde PN, Fell B, Dickerson R, Stoner JT, Kackley ML, Crabtree CD, Decker DD, et al. Feasibility and metabolic outcomes of a well-formulated ketogenic diet as an adjuvant therapeutic intervention for women with stage IV metastatic breast cancer: The Keto-CARE trial. PLoS ONE. 2024;19(1): e0296523.
Seyfried TN, Arismendi-Morillo G, Mukherjee P, Chinopoulos C: On the Origin of ATP Synthesis in Cancer. iScience 2020, 23(11):101761.
Maroon JC, Seyfried TN, Donohue JP, Bost J. The role of metabolic therapy in treating glioblastoma multiforme. Surg Neurol Int. 2015;6:61.
Chang HT, Olson LK, Schwartz KA. Ketolytic and glycolytic enzymatic expression profiles in malignant gliomas: implication for ketogenic diet therapy. Nutr Metab (Lond). 2013;10(1):47.
Udumula MP, Singh H, Faraz R, Poisson L, Tiwari N, Dimitrova I, Hijaz M, Gogoi R, Swenor M, Munkarah A et al: Intermittent Fasting induced ketogenesis inhibits mouse epithelial ovarian tumors by promoting anti-tumor T cell response. bioRxiv 2023:2023.2003. 2008.531740.
Scheck AC, Abdelwahab MG, Fenton KE, Stafford P. The ketogenic diet for the treatment of glioma: insights from genetic profiling. Epilepsy Res. 2012;100(3):327–37.
Stafford P, Abdelwahab MG, Kim DY, Preul MC, Rho JM, Scheck AC. The ketogenic diet reverses gene expression patterns and reduces reactive oxygen species levels when used as an adjuvant therapy for glioma. Nutr Metab (Lond). 2010;7(1):74.
Mukherjee P, Mulrooney TJ, Marsh J, Blair D, Chiles TC, Seyfried TN. Differential effects of energy stress on AMPK phosphorylation and apoptosis in experimental brain tumor and normal brain. Mol Cancer. 2008;7:37.
Mulrooney TJ, Marsh J, Urits I, Seyfried TN, Mukherjee P. Influence of caloric restriction on constitutive expression of NF-kappaB in an experimental mouse astrocytoma. PLoS ONE. 2011;6(3): e18085.
Shelton LM, Huysentruyt LC, Mukherjee P, Seyfried TN. Calorie restriction as an anti-invasive therapy for malignant brain cancer in the VM mouse. ASN Neuro. 2010;2(3): e00038.
Zhou W, Mukherjee P, Kiebish MA, Markis WT, Mantis JG, Seyfried TN. The calorically restricted ketogenic diet, an effective alternative therapy for malignant brain cancer. Nutr Metab (Lond). 2007;4:5.
Mukherjee P, El-Abbadi MM, Kasperzyk JL, Ranes MK, Seyfried TN. Dietary restriction reduces angiogenesis and growth in an orthotopic mouse brain tumour model. Br J Cancer. 2002;86(10):1615–21.
Woolf EC, Curley KL, Liu Q, Turner GH, Charlton JA, Preul MC, Scheck AC. The Ketogenic Diet Alters the Hypoxic Response and Affects Expression of Proteins Associated with Angiogenesis, Invasive Potential and Vascular Permeability in a Mouse Glioma Model. PLoS ONE. 2015;10(6): e0130357.
Veech RL, Todd King M, Pawlosky R, Kashiwaya Y, Bradshaw PC, Curtis W. The “great” controlling nucleotide coenzymes. IUBMB Life. 2019;71(5):565–79.
Veech RL. The therapeutic implications of ketone bodies: the effects of ketone bodies in pathological conditions: ketosis, ketogenic diet, redox states, insulin resistance, and mitochondrial metabolism. Prostaglandins Leukot Essent Fatty Acids. 2004;70(3):309–19.
Seyfried TN, Arismendi-Morillo G, Zuccoli G, Lee DC, Duraj T, Elsakka AM, Maroon JC, Mukherjee P, Ta L, Shelton L, et al. Metabolic management of microenvironment acidity in glioblastoma. Front Oncol. 2022;12: 968351.
Liberti MV, Locasale JW. The Warburg effect: how does it benefit cancer cells? Trends Biochem Sci. 2016;41(3):211–8.
Wise DR, Thompson CB. Glutamine addiction: a new therapeutic target in cancer. Trends Biochem Sci. 2010;35(8):427–33.
Seyfried TN, Yu G, Maroon JC, D’Agostino DP. Press-pulse: a novel therapeutic strategy for the metabolic management of cancer. Nutr Metab (Lond). 2017;14:19.
Klement RJ. Beneficial effects of ketogenic diets for cancer patients: a realist review with focus on evidence and confirmation. Med Oncol. 2017;34(8):132.
Seyfried TN, Shivane AG, Kalamian M, Maroon JC, Mukherjee P, Zuccoli G. Ketogenic Metabolic Therapy, Without Chemo or Radiation, for the Long-Term Management of IDH1-Mutant Glioblastoma: An 80-Month Follow-Up Case Report. Front Nutr. 2021;8: 682243.
Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM, Fantin VR, Jang HG, Jin S, Keenan MC, et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2009;462(7274):739–44.
Fack F, Tardito S, Hochart G, Oudin A, Zheng L, Fritah S, Golebiewska A, Nazarov PV, Bernard A, Hau AC, et al. Altered metabolic landscape in IDH-mutant gliomas affects phospholipid, energy, and oxidative stress pathways. EMBO Mol Med. 2017;9(12):1681–95.
van Noorden CJF, Hira VVV, van Dijck AJ, Novak M, Breznik B, Molenaar RJ. Energy Metabolism in IDH1 Wild-Type and IDH1-Mutated Glioblastoma Stem Cells: A Novel Target for Therapy? Cells. 2021;10(3):705.
Chesnelong C, Chaumeil MM, Blough MD, Al-Najjar M, Stechishin OD, Chan JA, Pieper RO, Ronen SM, Weiss S, Luchman HA, et al. Lactate dehydrogenase A silencing in IDH mutant gliomas. Neuro Oncol. 2014;16(5):686–95.
Xu W, Yang H, Liu Y, Yang Y, Wang P, Kim S-H, Ito S, Yang C, Wang P, Xiao M-T. Oncometabolite 2-hydroxyglutarate is a competitive inhibitor of α-ketoglutarate-dependent dioxygenases. Cancer Cell. 2011;19(1):17–30.
Garcia CR, Highsmith KN, Knight S, Puduvalli VK, Kamiya-Matsuoka C. Single center experience of IDH inhibitors in high-grade gliomas. In.: American Society of Clinical Oncology; 2024.
Mellinghoff IK, Ellingson BM, Touat M, Maher E, De La Fuente MI, Holdhoff M, Cote GM, Burris H, Janku F, Young RJ. Ivosidenib in isocitrate dehydrogenase 1–mutated advanced glioma. J Clin Oncol. 2020;38(29):3398–406.
Kayabolen A, Yilmaz E, Bagci-Onder T. IDH Mutations in Glioma: Double-Edged Sword in Clinical Applications? Biomedicines. 2021;9(7):799.
Mukherjee P, Augur ZM, Li M, Hill C, Greenwood B, Domin MA, Kondakci G, Narain NR, Kiebish MA, Bronson RT, et al. Therapeutic benefit of combining calorie-restricted ketogenic diet and glutamine targeting in late-stage experimental glioblastoma. Commun Biol. 2019;2:200.
Javier R, Wang W, Drumm M, McCortney K, Sarkaria JN. Horbinski CJPo: The efficacy of an unrestricted cycling ketogenic diet in preclinical models of IDH wild-type and IDH mutant glioma. 2022;17(2): e0257725.
Phillips MCL, Leyden J, McManus EJ, Lowyim DG, Ziad F, Moon BG. Haji Mohd Yasin NAB, Tan A, Thotathil Z, Jameson MB: Feasibility and Safety of a Combined Metabolic Strategy in Glioblastoma Multiforme: A Prospective Case Series. Journal of oncology. 2022;2022:4496734.
Nencioni A, Caffa I, Cortellino S, Longo VD. Fasting and cancer: molecular mechanisms and clinical application. Nat Rev Cancer. 2018;18(11):707–19.
Deligiorgi MV, Liapi C, Trafalis DT. How far are we from prescribing fasting as anticancer medicine? Int J Mol Sci. 2020;21(23):9175.
Harris AL. Development of cancer metabolism as a therapeutic target: New pathways, patient studies, stratification and combination therapy. Br J Cancer. 2020;122(1):1–3.
Menyhart O, Gyorffy B. Dietary approaches for exploiting metabolic vulnerabilities in cancer. Biochim Biophys Acta Rev Cancer. 2024;1879(2): 189062.
Klement RJ: Anti-tumor effects of ketogenic diets and their synergism with other treatments in mice: Bayesian evidence synthesis of 1755 individual mouse survival data. Biomed J 2023:100609.
Xia S, Lin R, Jin L, Zhao L, Kang HB, Pan Y, Liu S, Qian G, Qian Z, Konstantakou E, et al. Prevention of Dietary-Fat-Fueled Ketogenesis Attenuates BRAF V600E Tumor Growth. Cell Metab. 2017;25(2):358–73.
Weber DD, Aminzadeh-Gohari S, Thapa M, Redtenbacher AS, Catalano L, Capeloa T, Vazeille T, Emberger M, Felder TK, Feichtinger RG, et al. Ketogenic diets slow melanoma growth in vivo regardless of tumor genetics and metabolic plasticity. Cancer Metab. 2022;10(1):12.
Guo A, Asztely F, Smits A, Jakola AS. Methodological Approaches to Ketogenic Dietary Treatments in Glioma Patients from a Nutritional Point of View. Nutr Cancer. 2023;75(1):112–22.
Supportive PDQ, Palliative Care Editorial B: Nutrition in Cancer Care (PDQ(R)): Health Professional Version. In: PDQ Cancer Information Summaries. edn. Bethesda (MD): National Cancer Institute (US); 2002.
Klement RJ, Brehm N, Sweeney RA. Ketogenic diets in medical oncology: a systematic review with focus on clinical outcomes. Med Oncol. 2020;37(2):14.
Lévesque S, Pol JG, Ferrere G, Galluzzi L, Zitvogel L, Kroemer G. Trial watch: dietary interventions for cancer therapy. Oncoimmunology. 2019;8(7): e1591878.
Lemberg KM, Gori SS, Tsukamoto T, Rais R, Slusher BS: Clinical development of metabolic inhibitors for oncology. J Clin Invest 2022, 132(1).
Zhu H, Bi D, Zhang Y, Kong C, Du J, Wu X, Wei Q, Qin H. Ketogenic diet for human diseases: the underlying mechanisms and potential for clinical implementations. Signal Transduct Target Ther. 2022;7(1):11.
Qin J, Huang X, Gou S, Zhang S, Gou Y, Zhang Q, Chen H, Sun L, Chen M, Liu D: Ketogenic diet reshapes cancer metabolism through lysine β-hydroxybutyrylation. Nature Metabolism 2024:1–24.
Luengo A, Li Z, Gui DY, Sullivan LB, Zagorulya M, Do BT, Ferreira R, Naamati A, Ali A, Lewis CA, et al. Increased demand for NAD(+) relative to ATP drives aerobic glycolysis. Mol Cell. 2021;81(4):691–707 e696.
Hensley CT, Wasti AT, DeBerardinis RJ. Glutamine and cancer: cell biology, physiology, and clinical opportunities. J Clin Invest. 2013;123(9):3678–84.
Smith KA, Hendricks BK, DiDomenico JD, Conway BN, Smith TL, Azadi A, Fonkem E. Ketogenic Metabolic Therapy for Glioma Cureus. 2022;14(6): e26457.
McDonald TJ, Cervenka MC: Ketogenic diet therapies for seizures and status epilepticus. In: Seminars in neurology: 2020: Thieme Medical Publishers, Inc. 333 Seventh Avenue, 18th Floor, New York, NY …; 2020: 719–729.
Scannell JW, Blanckley A, Boldon H, Warrington B. Diagnosing the decline in pharmaceutical R&D efficiency. Nat Rev Drug Discov. 2012;11(3):191–200.
Emmerich CH, Gamboa LM, Hofmann MCJ, Bonin-Andresen M, Arbach O, Schendel P, Gerlach B, Hempel K, Bespalov A, Dirnagl U, et al. Improving target assessment in biomedical research: the GOT-IT recommendations. Nat Rev Drug Discov. 2021;20(1):64–81.
Scheck AC, Abdelwahab MG, Fenton K, Stafford P. The ketogenic diet for the treatment of glioma: Insights from genetic profiling. Epilepsy Res. 2012;100:327–37.
Lussier DM, Woolf EC, Johnson JL, Brooks KS, Blattman JN, Scheck AC. Enhanced immunity in a mouse model of malignant glioma is mediated by a therapeutic ketogenic diet. BMC Cancer. 2016;16:310.
Scheck AC, Syed N: Ketogenic Diet as an Adjunctuive Therapy for Malignant Brain Cancer. In: Ketogenic Diet and Metabolic Therapies: Expanded Roles in Health and Disease 2nd Edition. edn. Edited by Masino SA, Boison D, D’Agostino DP, Kossoff EH, Rho JM. New York: Oxford University Press; 2022: 125–153.
Maeyama M, Tanaka K, Nishihara M, Irino Y, Shinohara M, Nagashima H, Tanaka H, Nakamizo S, Hashiguchi M, Fujita Y, et al. Metabolic changes and anti-tumor effects of a ketogenic diet combined with anti-angiogenic therapy in a glioblastoma mouse model. Sci Rep. 2021;11(1):79.
Ferrere G, Tidjani Alou M, Liu P, Goubet AG, Fidelle M, Kepp O, Durand S, Iebba V, Fluckiger A, Daillere R et al: Ketogenic diet and ketone bodies enhance the anticancer effects of PD-1 blockade. JCI Insight 2021, 6(2).
Miller VJ, Villamena FA, Volek JS. Nutritional Ketosis and Mitohormesis: Potential Implications for Mitochondrial Function and Human Health. J Nutr Metab. 2018;2018:5157645.
Talib WH, Mahmod AI, Kamal A, Rashid HM, Alashqar AMD, Khater S, Jamal D, Waly M. Ketogenic Diet in Cancer Prevention and Therapy: Molecular Targets and Therapeutic Opportunities. Curr Issues Mol Biol. 2021;43(2):558–89.
Romer M, Dorfler J, Huebner J. The use of ketogenic diets in cancer patients: a systematic review. Clin Exp Med. 2021;21(4):501–36.
Meidenbauer JJ, Mukherjee P, Seyfried TN. The glucose ketone index calculator: a simple tool to monitor therapeutic efficacy for metabolic management of brain cancer. Nutr Metab (Lond). 2015;12(1):12.
Evangeliou AE, Spilioti MG, Vassilakou D, Goutsaridou F, Seyfried TN. Restricted Ketogenic Diet Therapy for Primary Lung Cancer With Metastasis to the Brain: A Case Report. Cureus. 2022;14(8): e27603.
Barroso I, McCarthy MI. The Genetic Basis of Metabolic Disease. Cell. 2019;177(1):146–61.
Zeevi D, Korem T, Zmora N, Israeli D, Rothschild D, Weinberger A, Ben-Yacov O, Lador D, Avnit-Sagi T, Lotan-Pompan M, et al. Personalized Nutrition by Prediction of Glycemic Responses. Cell. 2015;163(5):1079–94.
Westman EC, Yancy WS Jr, Humphreys M. Dietary treatment of diabetes mellitus in the pre-insulin era (1914–1922). Perspect Biol Med. 2006;49(1):77–83.
Freeman JM, Kossoff EH. Ketosis and the ketogenic diet, 2010: advances in treating epilepsy and other disorders. Adv Pediatr. 2010;57(1):315–29.
Roehl K, Falco-Walter J, Ouyang B, Balabanov A. Modified ketogenic diets in adults with refractory epilepsy: Efficacious improvements in seizure frequency, seizure severity, and quality of life. Epilepsy Behav. 2019;93:113–8.
Scholl-Bürgi S, Höller A, Pichler K, Michel M, Haberlandt E, Karall D. Ketogenic diets in patients with inherited metabolic disorders. J Inherit Metab Dis. 2015;38:765–73.
Paoli A, Rubini A, Volek JS, Grimaldi KA. Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. Eur J Clin Nutr. 2013;67(8):789–96.
Sarnyai Z, Palmer CM. Ketogenic Therapy in Serious Mental Illness: Emerging Evidence. Int J Neuropsychopharmacol. 2020;23(7):434–9.
Klement RJ. Wilhelm Brünings’ forgotten contribution to the metabolic treatment of cancer utilizing hypoglycemia and a very low carbohydrate (ketogenic) diet. Journal of traditional Complementary Medicine. 2019;9(3):192–200.
Morris AA. Cerebral ketone body metabolism. J Inherit Metab Dis. 2005;28(2):109–21.
Robinson AM, Williamson DH. Physiological roles of ketone bodies as substrates and signals in mammalian tissues. Physiol Rev. 1980;60(1):143–87.
Musa-Veloso K, Likhodii SS, Cunnane SC. Breath acetone is a reliable indicator of ketosis in adults consuming ketogenic meals. Am J Clin Nutr. 2002;76(1):65–70.
Krebs H, Williamson D, Bates MW, Page MA, Hawkins R. The role of ketone bodies in caloric homeostasis. Adv Enzyme Regul. 1971;9:387–409.
Rui L. Energy metabolism in the liver. Compr Physiol. 2014;4(1):177–97.
White H, Venkatesh B. Clinical review: ketones and brain injury. Crit Care. 2011;15(2):219.
LaManna JC, Salem N, Puchowicz M, Erokwu B, Koppaka S, Flask C, Lee Z: Ketones suppress brain glucose consumption. In: Oxygen Transport to Tissue XXX. edn.: Springer; 2009: 301–306.
Owen OE, Morgan AP, Kemp HG, Sullivan JM, Herrera MG, Cahill GF Jr. Brain metabolism during fasting. J Clin Invest. 1967;46(10):1589–95.
Laffel L. Ketone bodies: a review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab Res Rev. 1999;15(6):412–26.
Fine EJ, Feinman RD. Insulin, carbohydrate restriction, metabolic syndrome and cancer. Expert Rev Endocrinol Metab. 2015;10(1):15–24.
Cooper ID, Brookler KH, Kyriakidou Y, Elliott BT, Crofts CAP. Metabolic Phenotypes and Step by Step Evolution of Type 2 Diabetes: A New Paradigm. Biomedicines. 2021;9(7):800.
Voss M, Wagner M, von Mettenheim N, Harter PN, Wenger KJ, Franz K, Bojunga J, Vetter M, Gerlach R, Glatzel M, et al. ERGO2: A Prospective, Randomized Trial of Calorie-Restricted Ketogenic Diet and Fasting in Addition to Reirradiation for Malignant Glioma. Int J Radiat Oncol Biol Phys. 2020;108(4):987–95.
Egashira R, Matsunaga M, Miyake A, Hotta S, Nagai N, Yamaguchi C, Takeuchi M, Moriguchi M, Tonari S, Nakano M, et al. Long-Term Effects of a Ketogenic Diet for Cancer. Nutrients. 2023;15(10):2334.
Purow B. For glioma, a sweet side to diabetes. Neuro Oncol. 2016;18(3):306–7.
Noch EK, Palma LN, Yim I, Bullen N, Qiu Y, Ravichandran H, Kim J, Rendeiro A, Davis MB, Elemento O, et al. Insulin feedback is a targetable resistance mechanism of PI3K inhibition in glioblastoma. Neuro Oncol. 2023;25(12):2165–76.
Yusuf S, Aretz P, Nickel AC, Westhoff P, Sharma A, Qin N, Remke M, Steiger HJ, Hanggi D, Liu H, et al. WNT/beta-Catenin-Mediated Resistance to Glucose Deprivation in Glioblastoma Stem-like Cells. Cancers (Basel). 2022;14(13):3165.
Yamaguchi I, Yoshimura SH, Katoh H. High cell density increases glioblastoma cell viability under glucose deprivation via degradation of the cystine/glutamate transporter xCT (SLC7A11). J Biol Chem. 2020;295(20):6936–45.
Bielecka-Wajdman AM, Ludyga T, Smyk D, Smyk W, Mularska M, Swiderek P, Majewski W, Mullins CS, Linnebacher M, Obuchowicz E. Glucose Influences the Response of Glioblastoma Cells to Temozolomide and Dexamethasone. Cancer Control. 2022;29:10732748221075468.
Cooper ID, Kyriakidou Y, Edwards K, Petagine L, Seyfried TN, Duraj T, Soto-Mota A, Scarborough A, Jacome SL, Brookler K, et al. Ketosis Suppression and Ageing (KetoSAge): The Effects of Suppressing Ketosis in Long Term Keto-Adapted Non-Athletic Females. Int J Mol Sci. 2023;24(21):15621.
Urbain P, Bertz H. Monitoring for compliance with a ketogenic diet: what is the best time of day to test for urinary ketosis? Nutrition metabolism. 2016;13(1):1–6.
Balasse EO, Fery F. Ketone body production and disposal: effects of fasting, diabetes, and exercise. Diabetes Metab Rev. 1989;5(3):247–70.
Owen OE, Hanson RW: Ketone Bodies. In: Encyclopedia of Endocrine Diseases. edn. Edited by Martini L. New York: Elsevier; 2004: 125–136.
Kossoff EH, Zupec-Kania BA, Auvin S, Ballaban-Gil KR, Christina Bergqvist AG, Blackford R, Buchhalter JR, Caraballo RH, Cross JH, Dahlin MG, et al. Optimal clinical management of children receiving dietary therapies for epilepsy: Updated recommendations of the International Ketogenic Diet Study Group. Epilepsia Open. 2018;3(2):175–92.
Cervenka MC, Wood S, Bagary M, Balabanov A, Bercovici E, Brown MG, Devinsky O, Di Lorenzo C, Doherty CP, Felton E, et al. International Recommendations for the Management of Adults Treated With Ketogenic Diet Therapies. Neurol Clin Pract. 2021;11(5):385–97.
Watanabe M, Tuccinardi D, Ernesti I, Basciani S, Mariani S, Genco A, Manfrini S, Lubrano C, Gnessi L. Scientific evidence underlying contraindications to the ketogenic diet: An update. Obes Rev. 2020;21(10): e13053.
Phinney SD, Volek JS: The art and science of low carbohydrate performance. In.: Beyond Obesity LLC, Miami, FL, USA; 2011.
Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51(2):241–7.
Barcellos PS, Borges N, Torres DPM. Resting energy expenditure in cancer patients: Agreement between predictive equations and indirect calorimetry. Clin Nutr ESPEN. 2021;42:286–91.
McDonald TJW, Cervenka MC. Ketogenic Diets for Adults With Highly Refractory Epilepsy. Epilepsy currents / American Epilepsy Society. 2017;17(6):346–50.
Martin-McGill KJ, Bresnahan R, Levy RG, Cooper PN. Ketogenic diets for drug-resistant epilepsy. Cochrane Database Syst Rev. 2020;6(6):CD001903.
Hagstrom H, Hagfors LN, Tellstrom A, Hedelin R, Lindmark K. Low carbohydrate high fat-diet in real life assessed by diet history interviews. Nutr J. 2023;22(1):14.
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, Fearon K, Hutterer E, Isenring E, Kaasa S, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36(1):11–48.
Capitao C, Coutinho D, Neves PM, Capelas ML, Pimenta NM, Santos T, Makitie A, Ravasco P. Protein intake and muscle mass maintenance in patients with cancer types with high prevalence of sarcopenia: a systematic review. Support Care Cancer. 2022;30(4):3007–15.
Tóth C, Dabóczi A, Chanrai M, Schimmer M, Clemens Z: 38-Month long progression-free and symptom-free survival of a patient with recurrent glioblastoma multiforme: a case report of the paleolithic ketogenic diet (Pkd) used as a stand-alone treatment after failed standard oncotherapy. 2019.
O’Hearn AJCOiE, Diabetes, Obesity: Can a carnivore diet provide all essential nutrients? 2020, 27(5):312–316.
Li J, Zhang H, Dai Z. Cancer Treatment With the Ketogenic Diet: A Systematic Review and Meta-analysis of Animal Studies. Front Nutr. 2021;8: 594408.
Weber DD, Aminzadeh-Gohari S, Tulipan J, Catalano L, Feichtinger RG, Kofler B. Ketogenic diet in the treatment of cancer–where do we stand? Molecular metabolism. 2020;33:102–21.
Porper K, Shpatz Y, Plotkin L, Pechthold RG, Talianski A, Champ CE, Furman O, Shimoni-Sebag A, Symon Z, Amit U, et al. A Phase I clinical trial of dose-escalated metabolic therapy combined with concomitant radiation therapy in high-grade glioma. J Neurooncol. 2021;153(3):487–96.
Lien EC, Westermark AM, Zhang Y, Yuan C, Li Z, Lau AN, Sapp KM, Wolpin BM, Vander Heiden MG. Low glycaemic diets alter lipid metabolism to influence tumour growth. Nature. 2021;599(7884):302–7.
Lv M, Zhu X, Wang H, Wang F, Guan W. Roles of caloric restriction, ketogenic diet and intermittent fasting during initiation, progression and metastasis of cancer in animal models: a systematic review and meta-analysis. PLoS ONE. 2014;9(12): e115147.
Zhou W, Mukherjee P, Kiebish MA, Markis WT. Mantis JG. Seyfried TNJN, metabolism: The calorically restricted ketogenic diet, an effective alternative therapy for malignant brain cancer. 2007;4(1):1–15.
Lu Y, Tao F, Zhou MT, Tang KF. The signaling pathways that mediate the anti-cancer effects of caloric restriction. Pharmacol Res. 2019;141:512–20.
Meynet O, Ricci JE. Caloric restriction and cancer: molecular mechanisms and clinical implications. Trends Mol Med. 2014;20(8):419–27.
Nencioni A, Caffa I, Cortellino S. Longo VDJNRC: Fasting and cancer: molecular mechanisms and clinical application. 2018;18(11):707–19.
Roekenes J, Martins C. Ketogenic diets and appetite regulation. Curr Opin Clin Nutr Metab Care. 2021;24(4):359–63.
Tisdale MJ, Brennan RA, Fearon KC. Reduction of weight loss and tumour size in a cachexia model by a high fat diet. Br J Cancer. 1987;56(1):39–43.
Klement RJ, Champ CE, Kämmerer U, Koebrunner PS, Krage K, Schäfer G, Weigel M, Sweeney RA. Impact of a ketogenic diet intervention during radiotherapy on body composition: III—final results of the KETOCOMP study for breast cancer patients. Breast Cancer Res. 2020;22:1–14.
Klement RJ, Koebrunner PS, Meyer D, Kanzler S, Sweeney RA: Impact of a ketogenic diet intervention during radiotherapy on body composition: IV. Final results of the KETOCOMP study for rectal cancer patients. Clin Nutr 2021, 40(7):4674–4684.
Shukla SK, Gebregiworgis T, Purohit V, Chaika NV, Gunda V, Radhakrishnan P, Mehla K, Pipinos II, Powers R, Yu F, et al. Metabolic reprogramming induced by ketone bodies diminishes pancreatic cancer cachexia. Cancer Metab. 2014;2(1):18.
Nakamura K, Tonouchi H, Sasayama A, Ashida K. A Ketogenic Formula Prevents Tumor Progression and Cancer Cachexia by Attenuating Systemic Inflammation in Colon 26 Tumor-Bearing Mice. Nutrients. 2018;10(2):206.
Koutnik AP, D’Agostino DP, Egan B. Anticatabolic Effects of Ketone Bodies in Skeletal Muscle. Trends Endocrinol Metab. 2019;30(4):227–9.
Koutnik AP, Poff AM, Ward NP, DeBlasi JM, Soliven MA, Romero MA, Roberson PA, Fox CD, Roberts MD, D’Agostino DP. Ketone Bodies Attenuate Wasting in Models of Atrophy. J Cachexia Sarcopenia Muscle. 2020;11(4):973–96.
Thomsen HH, Rittig N, Johannsen M, Moller AB, Jorgensen JO, Jessen N, Moller N. Effects of 3-hydroxybutyrate and free fatty acids on muscle protein kinetics and signaling during LPS-induced inflammation in humans: anticatabolic impact of ketone bodies. Am J Clin Nutr. 2018;108(4):857–67.
Youm Y-H, Nguyen KY, Grant RW, Goldberg EL, Bodogai M, Kim D, D’agostino D, Planavsky N, Lupfer C, Kanneganti TD. The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome–mediated inflammatory disease. Nat Med. 2015;21(3):263–9.
Fromentin C, Tome D, Nau F, Flet L, Luengo C, Azzout-Marniche D, Sanders P, Fromentin G, Gaudichon C. Dietary proteins contribute little to glucose production, even under optimal gluconeogenic conditions in healthy humans. Diabetes. 2013;62(5):1435–42.
Sharma R, Tiwari S. Renal gluconeogenesis in insulin resistance: A culprit for hyperglycemia in diabetes. World J Diabetes. 2021;12(5):556–68.
Pillot B, Soty M, Gautier-Stein A, Zitoun C, Mithieux G. Protein feeding promotes redistribution of endogenous glucose production to the kidney and potentiates its suppression by insulin. Endocrinology. 2009;150(2):616–24.
Hudson JL, Wang Y, Bergia Iii RE, Campbell WW. Protein Intake Greater than the RDA Differentially Influences Whole-Body Lean Mass Responses to Purposeful Catabolic and Anabolic Stressors: A Systematic Review and Meta-analysis. Adv Nutr. 2020;11(3):548–58.
Trumbo P, Schlicker S, Yates A, Poos M: Food and Nutrition Board of the Institute of Medicine, The National Academies. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc 2002, 102(11):1621–1630.
Richter M, Baerlocher K, Bauer JM, Elmadfa I, Heseker H, Leschik-Bonnet E, Stangl G, Volkert D, Stehle P. on behalf of the German Nutrition S: Revised Reference Values for the Intake of Protein. Ann Nutr Metab. 2019;74(3):242–50.
Bergstrom J, Furst P, Noree LO, Vinnars E. Intracellular free amino acid concentration in human muscle tissue. J Appl Physiol. 1974;36(6):693–7.
Cruzat V, Macedo Rogero M, Noel Keane K, Curi R, Newsholme P. Glutamine: Metabolism and Immune Function, Supplementation and Clinical Translation. Nutrients. 2018;10(11):1564.
Gleeson M, Blannin AK, Walsh NP, Bishop NC, Clark AM. Effect of low- and high-carbohydrate diets on the plasma glutamine and circulating leukocyte responses to exercise. Int J Sport Nutr. 1998;8(1):49–59.
Aoki TT, Muller WA, Cahill GF Jr. Hormonal regulation of glutamine metabolism in fasting man. Adv Enzyme Regul. 1972;10:145–51.
Pedersen KS, Gatto F, Zerahn B, Nielsen J, Pedersen BK, Hojman P, Gehl J: Exercise-Mediated Lowering of Glutamine Availability Suppresses Tumor Growth and Attenuates Muscle Wasting. iScience 2020, 23(4):100978.
Walsh NP, Blannin AK, Robson PJ, Gleeson M. Glutamine, exercise and immune function Links and possible mechanisms. Sports Med. 1998;26(3):177–91.
St-Pierre V, Vandenberghe C, Lowry CM, Fortier M, Castellano CA, Wagner R, Cunnane SC. Plasma Ketone and Medium Chain Fatty Acid Response in Humans Consuming Different Medium Chain Triglycerides During a Metabolic Study Day. Front Nutr. 2019;6:46.
Altinoz MA, Ozpinar A, Seyfried TN. Caprylic (Octanoic) Acid as a Potential Fatty Acid Chemotherapeutic for Glioblastoma. Prostaglandins Leukot Essent Fatty Acids. 2020;159: 102142.
Liu YM. Medium-chain triglyceride (MCT) ketogenic therapy. Epilepsia. 2008;49(Suppl 8):33–6.
Nebeling LC, Lerner E. Implementing a ketogenic diet based on medium-chain triglyceride oil in pediatric patients with cancer. J Am Diet Assoc. 1995;95(6):693–7.
Martin-McGill KJ, Marson AG, Tudur Smith C, Young B, Mills SJ, Cherry MG, Jenkinson MD. Ketogenic diets as an adjuvant therapy for glioblastoma (KEATING): a randomized, mixed methods, feasibility study. J Neurooncol. 2020;147(1):213–27.
van der Louw EJ, Olieman JF, van den Bemt PM, Bromberg JE, Oomen-de Hoop E, Neuteboom RF, Catsman-Berrevoets CE, Vincent AJ. Ketogenic diet treatment as adjuvant to standard treatment of glioblastoma multiforme: a feasibility and safety study. Therapeutic advances in medical oncology. 2019;11:1758835919853958.
Khodabakhshi A, Akbari ME, Mirzaei HR, Mehrad-Majd H, Kalamian M, Davoodi SH. Feasibility, Safety, and Beneficial Effects of MCT-Based Ketogenic Diet for Breast Cancer Treatment: A Randomized Controlled Trial Study. Nutr Cancer. 2020;72(4):627–34.
Lindeberg S: Modern Human Physiology with Respect to Evolutionary Adaptations that Relate to Diet in the Past. Evolution of Hominin Diets 2009:43–57.
Gibson RS, Raboy V, King JC. Implications of phytate in plant-based foods for iron and zinc bioavailability, setting dietary requirements, and formulating programs and policies. Nutr Rev. 2018;76(11):793–804.
Norton SK: Lost seasonality and overconsumption of plants: Risking oxalate toxicity. Journal of Evolution Health: A joint publication of the Ancestral Health Society the Society for Evolutionary Medicine Health 2017, 2(3).
Nath H, Samtiya M, Dhewa T. Beneficial attributes and adverse effects of major plant-based foods anti-nutrients on health: A review. Human Nutrition & Metabolism. 2022;28: 200147.
Poff AM, Koutnik AP, Egan B. Nutritional Ketosis with Ketogenic Diets or Exogenous Ketones: Features, Convergence, and Divergence. Curr Sports Med Rep. 2020;19(7):251–9.
Nelson AB, Queathem ED, Puchalska P, Crawford PA. Metabolic Messengers: ketone bodies. Nat Metab. 2023;5(12):2062–74.
Dmitrieva-Posocco O, Wong AC, Lundgren P, Golos AM, Descamps HC, Dohnalova L, Cramer Z, Tian Y, Yueh B, Eskiocak O, et al. beta-Hydroxybutyrate suppresses colorectal cancer. Nature. 2022;605(7908):160–5.
Poff A, Koutnik AP, Egan KM, Sahebjam S, D’Agostino D, Kumar NB: Targeting the Warburg effect for cancer treatment: Ketogenic diets for management of glioma. In: Seminars in Cancer Biology: 2019: Elsevier; 2019: 135–148.
Poff AM, Ari C, Arnold P, Seyfried TN, D’Agostino DP. Ketone supplementation decreases tumor cell viability and prolongs survival of mice with metastatic cancer. Int J Cancer. 2014;135(7):1711–20.
Vallejo FA, Shah SS, de Cordoba N, Walters WM, Prince J, Khatib Z, Komotar RJ, Vanni S, Graham RM. The contribution of ketone bodies to glycolytic inhibition for the treatment of adult and pediatric glioblastoma. J Neurooncol. 2020;147(2):317–26.
Poff AM, Ward N, Seyfried TN, Arnold P, D’Agostino DP. Non-Toxic Metabolic Management of Metastatic Cancer in VM Mice: Novel Combination of Ketogenic Diet, Ketone Supplementation, and Hyperbaric Oxygen Therapy. PLoS ONE. 2015;10(6): e0127407.
White H, Heffernan AJ, Worrall S, Grunsfeld A, Thomas M: A Systematic Review of Intravenous β-Hydroxybutyrate Use in Humans–A Promising Future Therapy? Front Med 2021:1611.
Cahill GF Jr. Fuel metabolism in starvation. Annu Rev Nutr. 2006;26:1–22.
Ari C, Murdun C, Koutnik AP, Goldhagen CR, Rogers C, Park C, Bharwani S, Diamond DM, Kindy MS, D’Agostino DP, et al. Exogenous Ketones Lower Blood Glucose Level in Rested and Exercised Rodent Models. Nutrients. 2019;11(10):2330.
Soto-Mota A, Norwitz NG, Evans RD, Clarke K. Exogenous d-β-hydroxybutyrate lowers blood glucose in part by decreasing the availability of L-alanine for gluconeogenesis. Endocrinology, Diabetes Metabolism. 2022;5(1): e00300.
Kesl SL, Poff AM, Ward NP, Fiorelli TN, Ari C, Van Putten AJ, Sherwood JW, Arnold P, D’Agostino DP. Effects of exogenous ketone supplementation on blood ketone, glucose, triglyceride, and lipoprotein levels in Sprague-Dawley rats. Nutr Metab (Lond). 2016;13(1):9.
Myette-Cote E, Neudorf H, Rafiei H, Clarke K, Little J. Prior ingestion of exogenous ketone monoester attenuates the glycaemic response to an oral glucose tolerance test in healthy young individuals. J Physiol. 2018:596(8):1385–95.
Myette-Cote E, Caldwell HG, Ainslie PN, Clarke K, Little JP. A ketone monoester drink reduces the glycemic response to an oral glucose challenge in individuals with obesity: a randomized trial. Am J Clin Nutr. 2019;110(6):1491–501.
Poff AM, Ari C, Seyfried TN, D’Agostino DP. The ketogenic diet and hyperbaric oxygen therapy prolong survival in mice with systemic metastatic cancer. PLoS ONE. 2013;8(6): e65522.
D’Agostino DP, Pilla R, Held HE, Landon CS, Puchowicz M, Brunengraber H, Ari C, Arnold P, Dean JB. Therapeutic ketosis with ketone ester delays central nervous system oxygen toxicity seizures in rats. Am J Physiol. 2013;304(10):R829–836.
Aminzadeh-Gohari S, Feichtinger RG, Vidali S, Locker F, Rutherford T, O’Donnel M, Stoger-Kleiber A, Mayr JA, Sperl W, Kofler B. A ketogenic diet supplemented with medium-chain triglycerides enhances the anti-tumor and anti-angiogenic efficacy of chemotherapy on neuroblastoma xenografts in a CD1-nu mouse model. Oncotarget. 2017;8(39):64728–44.
Iyikesici MS. Long-Term Survival Outcomes of Metabolically Supported Chemotherapy with Gemcitabine-Based or FOLFIRINOX Regimen Combined with Ketogenic Diet, Hyperthermia, and Hyperbaric Oxygen Therapy in Metastatic Pancreatic Cancer. Complement Med Res. 2020;27(1):31–9.
Curtis W, Kemper M, Miller A, Pawlosky R, King MT, Veech R: Mitigation of damage from reactive oxygen species and ionizing radiation by ketone body esters: Oxford University Press, New York, NY; 2017.
Roehl K, Sewak SL. Practice Paper of the Academy of Nutrition and Dietetics: Classic and Modified Ketogenic Diets for Treatment of Epilepsy. J Acad Nutr Diet. 2017;117(8):1279–92.
Johnstone AM, Horgan GW, Murison SD, Bremner DM, Lobley GE. Effects of a high-protein ketogenic diet on hunger, appetite, and weight loss in obese men feeding ad libitum. Am J Clin Nutr. 2008;87(1):44–55.
Tóth C, Clemens Z. Treatment of rectal cancer with the paleolithic ketogenic diet: a 24-months follow-up. Am J Med Case Reports. 2017;5(8):205–16.
Paoli A, Cenci L, Grimaldi KA. Effect of ketogenic Mediterranean diet with phytoextracts and low carbohydrates/high-protein meals on weight, cardiovascular risk factors, body composition and diet compliance in Italian council employees. Nutr J. 2011;10(1):112.
Ferraris C, Guglielmetti M, Neri LCL, Allehdan S, Mohsin Albasara JM, Fareed Alawadhi HH, Trentani C, Perna S, Tagliabue A. A Review of Ketogenic Dietary Therapies for Epilepsy and Neurological Diseases: A Proposal to Implement an Adapted Model to Include Healthy Mediterranean Products. Foods. 2023;12(9):1743.
Kirkpatrick CF, Bolick JP, Kris-Etherton PM, Sikand G, Aspry KE, Soffer DE, Willard KE, Maki KC: Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: A scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force. J Clin Lipidol 2019, 13(5):689–711 e681.
Jenkins DJ, Wong JM, Kendall CW, Esfahani A, Ng VW, Leong TC, Faulkner DA, Vidgen E, Paul G, Mukherjea R, et al. Effect of a 6-month vegan low-carbohydrate (‘Eco-Atkins’) diet on cardiovascular risk factors and body weight in hyperlipidaemic adults: a randomised controlled trial. BMJ Open. 2014;4(2): e003505.
Shilpa J, Mohan V. Ketogenic diets: Boon or bane? Indian J Med Res. 2018;148(3):251–3.
Brandhorst S. Fasting and fasting-mimicking diets for chemotherapy augmentation. Geroscience. 2021;43(3):1201–16.
Taylor SR, Falcone JN, Cantley LC, Goncalves MD. Developing dietary interventions as therapy for cancer. Nat Rev Cancer. 2022;22(8):452–66.
Jong CJ, Sandal P, Schaffer SW. The Role of Taurine in Mitochondria Health: More Than Just an Antioxidant. Molecules. 2021;26(16):4913.
Groesbeck DK, Bluml RM, Kossoff EH. Long-term use of the ketogenic diet in the treatment of epilepsy. Dev Med Child Neurol. 2006;48(12):978–81.
Batch JT, Lamsal SP, Adkins M, Sultan S, Ramirez MN. Advantages and Disadvantages of the Ketogenic Diet: A Review Article. Cureus. 2020;12(8): e9639.
Lindefeldt M, Eng A, Darban H, Bjerkner A, Zetterstrom CK, Allander T, Andersson B, Borenstein E, Dahlin M, Prast-Nielsen S. The ketogenic diet influences taxonomic and functional composition of the gut microbiota in children with severe epilepsy. NPJ Biofilms Microbiomes. 2019;5(1):5.
McNally MA, Pyzik PL, Rubenstein JE, Hamdy RF, Kossoff EH. Empiric use of potassium citrate reduces kidney-stone incidence with the ketogenic diet. Pediatrics. 2009;124(2):e300–304.
De Vivo DC, Bohan TP, Coulter DL, Dreifuss FE, Greenwood RS, Nordli DR Jr, Shields WD, Stafstrom CE, Tein I. L-carnitine supplementation in childhood epilepsy: current perspectives. Epilepsia. 1998;39(11):1216–25.
Lean ME, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, Peters C, Zhyzhneuskaya S, Al-Mrabeh A, Hollingsworth KG, et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet. 2018;391(10120):541–51.
Yeboah J, Young R, McClelland RL, Delaney JC, Polonsky TS, Dawood FZ, Blaha MJ, Miedema MD, Sibley CT, Carr JJ, et al. Utility of Nontraditional Risk Markers in Atherosclerotic Cardiovascular Disease Risk Assessment. J Am Coll Cardiol. 2016;67(2):139–47.
Hallberg SJ, McKenzie AL, Williams PT, Bhanpuri NH, Peters AL, Campbell WW, Hazbun TL, Volk BM, McCarter JP, Phinney SD. Effectiveness and safety of a novel care model for the management of type 2 diabetes at 1 year: an open-label, non-randomized, controlled study. Diabetes Therapy. 2018;9(2):583–612.
Yetley EA, DeMets DL, Harlan WR Jr. Surrogate disease markers as substitutes for chronic disease outcomes in studies of diet and chronic disease relations. Am J Clin Nutr. 2017;106(5):1175–89.
Klein KR, Walker CP, McFerren AL, Huffman H, Frohlich F, Buse JB. Carbohydrate Intake Prior to Oral Glucose Tolerance Testing. J Endocr Soc. 2021;5(5):bvab049.
Cao J, Lei S, Wang X, Cheng S. The Effect of a Ketogenic Low-Carbohydrate, High-Fat Diet on Aerobic Capacity and Exercise Performance in Endurance Athletes: A Systematic Review and Meta-Analysis. Nutrients. 2021;13(8):2896.
Rodbard D. Continuous Glucose Monitoring: A Review of Recent Studies Demonstrating Improved Glycemic Outcomes. Diabetes Technol Ther. 2017;19(S3):S25–37.
Yost O, DeJonckheere M, Stonebraker S, Ling G, Buis L, Pop-Busui R, Kim N, Mizokami-Stout K, Richardson C. Continuous Glucose Monitoring With Low-Carbohydrate Diet Coaching in Adults With Prediabetes: Mixed Methods Pilot Study. JMIR Diabetes. 2020;5(4): e21551.
Nguyen KT, Xu NY, Zhang JY, Shang T, Basu A, Bergenstal RM, Castorino K, Chen KY, Kerr D, Koliwad SK, et al. Continuous Ketone Monitoring Consensus Report 2021. J Diabetes Sci Technol. 2022;16(3):689–715.
SIBIONICS to Make Debut at the 59th Annual Meeting of the European Association for the Study of Diabetes (EASD). In: PR Newswire Europe. 2023: NA.
Alva S, Brazg R, Castorino K, Kipnes M, Liljenquist DR, Liu H. Accuracy of the Third Generation of a 14-Day Continuous Glucose Monitoring System. Diabetes Ther. 2023;14(4):767–76.
Alva S, Castorino K, Cho H, Ou J. Feasibility of Continuous Ketone Monitoring in Subcutaneous Tissue Using a Ketone Sensor. J Diabetes Sci Technol. 2021;15(4):768–74.
Toth C, Clemens Z. Halted Progression of Soft Palate Cancer in a Patient Treated with the Paleolithic Ketogenic Diet Alone: A 20-months Follow-up. American Journal of Medical Case Reports. 2016;4(8):288–92.
Yakupova EI, Bocharnikov AD, Plotnikov EY. Effects of Ketogenic Diet on Muscle Metabolism in Health and Disease. Nutrients. 2022;14(18):3842.
Kalamian M: KETO for CANCER: Ketogenic Metabolic Therapy as a Targeted Nutritional Strategy. White River Junction, VT: Chelsea Green; 2017.
van Vliet S, Burd NA, van Loon LJ. The skeletal muscle anabolic response to plant-versus animal-based protein consumption. J Nutr. 2015;145(9):1981–91.
Shin E, Kang H, Lee H, Lee S, Jeon J, Seong K, Youn H, Youn B: Exosomal Plasminogen Activator Inhibitor-1 Induces Ionizing Radiation-Adaptive Glioblastoma Cachexia. Cells 2022, 11(19).
Sizoo EM, Braam L, Postma TJ, Pasman HR, Heimans JJ, Klein M, Reijneveld JC, Taphoorn MJ. Symptoms and problems in the end-of-life phase of high-grade glioma patients. Neuro Oncol. 2010;12(11):1162–6.
Furtner J, Genbrugge E, Gorlia T, Bendszus M, Nowosielski M, Golfinopoulos V, Weller M, Van Den Bent MJ, Wick W, Preusser M. Temporal muscle thickness is an independent prognostic marker in patients with progressive glioblastoma: translational imaging analysis of the EORTC 26101 trial. Neuro Oncol. 2019;21(12):1587–94.
Cui P, Shao W, Huang C, Wu CJ, Jiang B, Lin D. Metabolic derangements of skeletal muscle from a murine model of glioma cachexia. Skelet Muscle. 2019;9(1):3.
Klement RJ, Sweeney RA: Impact of a ketogenic diet intervention during radiotherapy on body composition: I. Initial clinical experience with six prospectively studied patients. BMC Res Notes 2016, 9:143.
Tomasin R, Martin ACBM, Cominetti MR. Metastasis and cachexia: alongside in clinics, but not so in animal models. J Cachexia Sarcopenia Muscle. 2019;10(6):1183–94.
Ferrer M, Mourikis N, Davidson EE, Kleeman SO, Zaccaria M, Habel J, Rubino R, Gao Q, Flint TR, Young L: Ketogenic diet promotes tumor ferroptosis but induces relative corticosterone deficiency that accelerates cachexia. Cell Metab 2023.
Cortez NE, Mackenzie GG. Ketogenic Diets in Pancreatic Cancer and Associated Cachexia: Cellular Mechanisms and Clinical Perspectives. Nutrients. 2021;13(9):3202.
van de Worp W, Schols A, Theys J, van Helvoort A, Langen RCJ. Nutritional Interventions in Cancer Cachexia: Evidence and Perspectives From Experimental Models. Front Nutr. 2020;7: 601329.
Setiawan T, Sari IN, Wijaya YT, Julianto NM, Muhammad JA, Lee H, Chae JH, Kwon HY. Cancer cachexia: molecular mechanisms and treatment strategies. J Hematol Oncol. 2023;16(1):54.
Christiansen AR, Lipshultz LI, Hotaling JM, Pastuszak AW. Selective androgen receptor modulators: the future of androgen therapy? Transl Androl Urol. 2020;9(Suppl 2):S135–48.
O’Hearn A. Can a carnivore diet provide all essential nutrients? Current Opinion in Endocrinology, Diabetes Obesity. 2020;27(5):312–6.
Churuangsuk C, Griffiths D, Lean MEJ, Combet E. Impacts of carbohydrate-restricted diets on micronutrient intakes and status: A systematic review. Obes Rev. 2019;20(8):1132–47.
Chu DY, Ravelli MN, Faltersack KM, Woods AL, Almane D, Li Z, Sampene E, Felton EA. Hypocarnitinemia and its effect on seizure control in adult patients with intractable epilepsy on the modified Atkins diet. Front Nutr. 2023;10:1304209.
Ferrara G, Kim J, Lin S, Hua J, Seto E. A Focused Review of Smartphone Diet-Tracking Apps: Usability, Functionality, Coherence With Behavior Change Theory, and Comparative Validity of Nutrient Intake and Energy Estimates. JMIR Mhealth Uhealth. 2019;7(5): e9232.
Chin SO, Keum C, Woo J, Park J, Choi HJ, Woo JT, Rhee SY. Successful weight reduction and maintenance by using a smartphone application in those with overweight and obesity. Sci Rep. 2016;6(1):34563.
Shah UA, Iyengar NM. Plant-Based and Ketogenic Diets As Diverging Paths to Address Cancer: A Review. JAMA Oncol. 2022;8(8):1201–8.
Ligibel JA, Bohlke K, May AM, Clinton SK, Demark-Wahnefried W, Gilchrist SC, Irwin ML, Late M, Mansfield S, Marshall TF. Exercise, diet, and weight management during cancer treatment: ASCO guideline. J Clin Oncol. 2022;40(22):2491–507.
Mittelman SD. The Role of Diet in Cancer Prevention and Chemotherapy Efficacy. Annu Rev Nutr. 2020;40:273–97.
Champ CE, Palmer JD, Volek JS, Werner-Wasik M, Andrews DW, Evans JJ, Glass J, Kim L, Shi W. Targeting metabolism with a ketogenic diet during the treatment of glioblastoma multiforme. J Neurooncol. 2014;117(1):125–31.
Seyfried TN, Flores R, Poff AM, D’Agostino DP, Mukherjee P: Metabolic therapy: a new paradigm for managing malignant brain cancer. Cancer Lett 2015, 356(2 Pt A):289–300.
Lane J, Brown NI, Williams S, Plaisance EP, Fontaine KR. Ketogenic Diet for Cancer: Critical Assessment and Research Recommendations. Nutrients. 2021;13(10):3562.
Yang YF, Mattamel PB, Joseph T, Huang J, Chen Q, Akinwunmi BO, Zhang CJP, Ming WK. Efficacy of Low-Carbohydrate Ketogenic Diet as an Adjuvant Cancer Therapy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2021;13(5):1388.
Arora N, Pulimamidi S, Yadav H, Jain S, Glover J, Dombrowski K, Hernandez B, Sarma AK, Aneja R. Intermittent fasting with ketogenic diet: A combination approach for management of chronic diseases. Clin Nutr ESPEN. 2023;54:166–74.
Phillips MCL, Thotathil Z, Dass PH, Ziad F, Moon BG. Ketogenic metabolic therapy in conjunction with standard treatment for glioblastoma: A case report. Oncol Lett. 2024;27(5):230.
Tian Q, Price ND, Hood L. Systems cancer medicine: towards realization of predictive, preventive, personalized and participatory (P4) medicine. J Intern Med. 2012;271(2):111–21.
Martinez-Garay C, Djouder N. Dietary interventions and precision nutrition in cancer therapy. Trends Mol Med. 2023;29(7):489–511.
Schwartz KA, Noel M, Nikolai M, Chang HT. Investigating the Ketogenic Diet As Treatment for Primary Aggressive Brain Cancer: Challenges and Lessons Learned. Front Nutr. 2018;5:11.
Blumenthal DT, Won M, Mehta MP, Curran WJ, Souhami L, Michalski JM, Rogers CL, Corn BW. Short delay in initiation of radiotherapy may not affect outcome of patients with glioblastoma: a secondary analysis from the radiation therapy oncology group database. J Clin Oncol. 2009;27(5):733–9.
Magrowski L, Nowicka E, Masri O, Tukiendorf A, Tarnawski R, Miszczyk M. The survival impact of significant delays between surgery and radiochemotherapy in glioblastoma patients: A retrospective analysis from a large tertiary center. J Clin Neurosci. 2021;90:39–47.
Zur I, Tzuk-Shina T, Guriel M, Eran A, Kaidar-Person O. Survival impact of the time gap between surgery and chemo-radiotherapy in glioblastoma patients. Sci Rep. 2020;10(1):1–10.
Sun MZ, Oh T, Ivan ME, Clark AJ, Safaee M, Sayegh ET, Kaur G, Parsa AT, Bloch O. Survival impact of time to initiation of chemoradiotherapy after resection of newly diagnosed glioblastoma. J Neurosurg. 2015;122(5):1144–50.
Katsigiannis S, Krischek B, Barleanu S, Grau S, Galldiks N, Timmer M, Kabbasch C, Goldbrunner R, Stavrinou P. Impact of time to initiation of radiotherapy on survival after resection of newly diagnosed glioblastoma. Radiat Oncol. 2019;14(1):73.
Zhang M, Xu F, Ni W, Qi W, Cao W, Xu C, Chen J, Gao Y. Survival impact of delaying postoperative chemoradiotherapy in newly-diagnosed glioblastoma patients. Transl Cancer Res. 2020;9(9):5450–8.
De Barros A, Attal J, Roques M, Nicolau J, Sol J-C, Cohen-Jonathan-Moyal E, Roux F-E. Impact on survival of early tumor growth between surgery and radiotherapy in patients with de novo glioblastoma. J Neurooncol. 2019;142:489–97.
Burnet NG, Jena R, Jefferies SJ, Stenning SP, Kirkby NF. Mathematical modelling of survival of glioblastoma patients suggests a role for radiotherapy dose escalation and predicts poorer outcome after delay to start treatment. Clin Oncol (R Coll Radiol). 2006;18(2):93–103.
Mellinghoff IK, van den Bent MJ, Blumenthal DT, Touat M, Peters KB, Clarke J, Mendez J, Yust-Katz S, Welsh L, Mason WP, et al. Vorasidenib in IDH1- or IDH2-Mutant Low-Grade Glioma. N Engl J Med. 2023;389(7):589–601.
Chaichana KL, Zadnik P, Weingart JD, Olivi A, Gallia GL, Blakeley J, Lim M, Brem H, Quinones-Hinojosa A. Multiple resections for patients with glioblastoma: prolonging survival. J Neurosurg. 2013;118(4):812–20.
Burnett T, Mozgunov P, Pallmann P, Villar SS, Wheeler GM, Jaki T. Adding flexibility to clinical trial designs: an example-based guide to the practical use of adaptive designs. BMC Med. 2020;18(1):352.
Pitre T, Cheng S, Cusano E, Khan N, Mikhail D, Leung G, Vernooij RWM, Yarnell CJ, Goligher E, Murthy S, et al. Methodology and design of platform trials: a meta-epidemiological study. J Clin Epidemiol. 2023;157:1–12.
Most MM, Ershow AG, Clevidence BA. An overview of methodologies, proficiencies, and training resources for controlled feeding studies. J Am Diet Assoc. 2003;103(6):729–35.
Cruwys T, Norwood R, Chachay VS, Ntontis E, Sheffield J. “An Important Part of Who I am”: The Predictors of Dietary Adherence among Weight-Loss, Vegetarian, Vegan, Paleo, and Gluten-Free Dietary Groups. Nutrients. 2020;12(4):970.
Kiessling L, Radbruch J, Schaube S: The impact of self-selection on performance. 2018.
Carrera PM, Kantarjian HM, Blinder VS. The financial burden and distress of patients with cancer: Understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J Clin. 2018;68(2):153–65.
Abrams HR, Durbin S, Huang CX, Johnson SF, Nayak RK, Zahner GJ, Peppercorn J. Financial toxicity in cancer care: origins, impact, and solutions. Transl Behav Med. 2021;11(11):2043–54.
Klement RJ, Weigel MM, Sweeney RA. A ketogenic diet consumed during radiotherapy improves several aspects of quality of life and metabolic health in women with breast cancer. Clin Nutr. 2021;40(6):4267–74.
Augustus E, Granderson I, Rocke KD. The Impact of a Ketogenic Dietary Intervention on the Quality of Life of Stage II and III Cancer Patients: A Randomized Controlled Trial in the Caribbean. Nutr Cancer. 2021;73(9):1590–600.
Tulipan J, Kofler B. Implementation of a Low-Carbohydrate Diet Improves the Quality of Life of Cancer Patients–An Online Survey. Front Nutr. 2021;8: 661253.
Kammerer U, Klement RJ, Joos FT, Sutterlin M, Reuss-Borst M. Low Carb and Ketogenic Diets Increase Quality of Life, Physical Performance, Body Composition, and Metabolic Health of Women with Breast Cancer. Nutrients. 2021;13(3):1029.
Chung VCH, Ho LTF, Leung TH, Wong CHL. Designing delivery models of traditional and complementary medicine services: a review of international experiences. Br Med Bull. 2021;137(1):70–81.
Lakomy R, Kazda T, Selingerova I, Poprach A, Pospisil P, Belanova R, Fadrus P, Vybihal V, Smrcka M, Jancalek R, et al. Real-World Evidence in Glioblastoma: Stupp’s Regimen After a Decade. Front Oncol. 2020;10:840.
Sheikh S, Radivoyevitch T, Barnholtz-Sloan JS, Vogelbaum M. Long-term trends in glioblastoma survival: implications for historical control groups in clinical trials. Neurooncol Pract. 2020;7(2):158–63.
Schork NJ. Personalized medicine: Time for one-person trials. Nature. 2015;520(7549):609–11.
Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, Kiene H, Helfand M, Altman DG, Sox H, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218–35.
Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D. The CARE guidelines: consensus-based clinical case reporting guideline development. Global advances in health medicine. 2013;2(5):38–43.
Vernieri C, Fuca G, Ligorio F, Huber V, Vingiani A, Iannelli F, Raimondi A, Rinchai D, Frige G, Belfiore A, et al. Fasting-Mimicking Diet Is Safe and Reshapes Metabolism and Antitumor Immunity in Patients with Cancer. Cancer Discov. 2022;12(1):90–107.
de Toledo FW, Grundler F, Bergouignan A, Drinda S, Michalsen A. Safety, health improvement and well-being during a 4 to 21-day fasting period in an observational study including 1422 subjects. PLoS ONE. 2019;14(1): e0209353.
Kreitzman SN, Coxon AY, Szaz KF. Glycogen storage: illusions of easy weight loss, excessive weight regain, and distortions in estimates of body composition. Am J Clin Nutr. 1992;56(1 Suppl):292S–293S.
Dai Z, Zhang H, Wu F, Chen Y, Yang C, Wang H, Sui X, Guo Y, Xin B, Guo Z, et al. Effects of 10-Day Complete Fasting on Physiological Homeostasis, Nutrition and Health Markers in Male Adults. Nutrients. 2022;14(18):3860.
Ogłodek E, Pilis P. Wiesław: Is Water-Only Fasting Safe? Global Advances in Health Medicine. 2021;10:21649561211031176.
Cuthbertson DJ, Steele T, Wilding JP, Halford J, Harrold JA, Hamer M, Karpe F. What have human experimental overfeeding studies taught us about adipose tissue expansion and susceptibility to obesity and metabolic complications? Int J Obes. 2017;41(6):853–65.
Fearon KC, Borland W, Preston T, Tisdale MJ, Shenkin A, Calman KC. Cancer cachexia: influence of systemic ketosis on substrate levels and nitrogen metabolism. Am J Clin Nutr. 1988;47(1):42–8.
Finnell JS, Saul BC, Goldhamer AC, Myers TR. Is fasting safe? A chart review of adverse events during medically supervised, water-only fasting. BMC complementary alternative medicine. 2018;18(1):1–9.
Valdemarin F, Caffa I, Persia A, Cremonini AL, Ferrando L, Tagliafico L, Tagliafico A, Guijarro A, Carbone F, Ministrini S, et al. Safety and Feasibility of Fasting-Mimicking Diet and Effects on Nutritional Status and Circulating Metabolic and Inflammatory Factors in Cancer Patients Undergoing Active Treatment. Cancers (Basel). 2021;13(16):4013.
Geurts M, van den Bent MJ. Timing of radiotherapy in newly diagnosed glioblastoma: no need to rush? Neuro Oncol. 2018;20(7):868–9.
Frenkel M. Refusing treatment. Oncologist. 2013;18(5):634–6.
Senderovitch H. The Ethical and Legal Dilemma in Terminating the Physician-Patient Relationship. Health Law Can. 2016;36(4):168–73.
Prabhakar A, Quach A, Zhang H, Terrera M, Jackemeyer D, Xian X, Tsow F, Tao N, Forzani ES. Acetone as biomarker for ketosis buildup capability–a study in healthy individuals under combined high fat and starvation diets. Nutr J. 2015;14(1):41.
Gibson AA, Eroglu EI, Rooney K, Harper C, McClintock S, Franklin J, Markovic TP, Seimon RV, Sainsbury A. Urine dipsticks are not accurate for detecting mild ketosis during a severely energy restricted diet. Obes Sci Pract. 2020;6(5):544–51.
Dalakleidi KV, Papadelli M, Kapolos I, Papadimitriou K. Applying Image-Based Food-Recognition Systems on Dietary Assessment: A Systematic Review. Adv Nutr. 2022;13(6):2590–619.
Tahir GA, Loo CK: A comprehensive survey of image-based food recognition and volume estimation methods for dietary assessment. In: Healthcare: 2021: Multidisciplinary Digital Publishing Institute; 2021: 1676.
Athinarayanan SJ, Adams RN, Hallberg SJ, McKenzie AL, Bhanpuri NH, Campbell WW, Volek JS, Phinney SD, McCarter JP. Long-Term Effects of a Novel Continuous Remote Care Intervention Including Nutritional Ketosis for the Management of Type 2 Diabetes: A 2-Year Non-randomized Clinical Trial. Front Endocrinol (Lausanne). 2019;10:348.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Hilliard ME, Isaacs D, Johnson EL: 1. Improving Care and Promoting Health in Populations: Standards of Care in Diabetes—2023. Diabetes Care 2023, 46(Supplement_1):S10-S18.
Masino SA: Ketogenic diet and metabolic therapies: expanded roles in health and disease: Oxford University Press; 2022.
Kossoff EH, Zahava Turner R, Cervenka MC, Barron BJ: Ketogenic Diet Therapies for Epilepsy and Other Conditions: Springer Publishing Company; 2020.
Attina A, Leggeri C, Paroni R, Pivari F, Dei Cas M, Mingione A, Dri M, Marchetti M, Di Renzo L. Fasting: How to Guide. Nutrients. 2021;13(5):1570.
Stafstrom CE, Rho JM: Epilepsy and the ketogenic diet: Springer Science & Business Media; 2004.
Volek J, Phinney SD, Kossoff E, Eberstein JA, Moore J: The Art and Science of Low Carbohydrate Living: An Expert Guide to Making the Life-saving Benefits of Carbohydrate Restriction Sustainable and Enjoyable: Beyond Obesity; 2011.
Bender JL, Babinski S, Wong G, Tricco AC, Englesakis M, Cyr AB, Potts H, Perski O, Esplen MJ, Young C, et al. Establishing best practices in cancer online support groups: protocol for a realist review. BMJ Open. 2021;11(11): e053916.
Young JS, Al-Adli N, Sibih YE, Scotford KL, Casey M, James S, Berger MS: Recognizing the psychological impact of a glioma diagnosis on mental and behavioral health: a systematic review of what neurosurgeons need to know. Journal of Neurosurgery 2022, 1(aop):1–9.
Tlusty G, Hanna KM. Health Ownership: A Concept Analysis. Nurs Sci Q. 2021;34(4):413–9.
Halatsch ME, Kast RE, Karpel-Massler G, Mayer B, Zolk O, Schmitz B, Scheuerle A, Maier L, Bullinger L, Mayer-Steinacker R et al: A phase Ib/IIa trial of 9 repurposed drugs combined with temozolomide for the treatment of recurrent glioblastoma: CUSP9v3. Neurooncol Adv 2021, 3(1):vdab075.
Agrawal S, Vamadevan P, Mazibuko N, Bannister R, Swery R, Wilson S, Edwards S. A New Method for Ethical and Efficient Evidence Generation for Off-Label Medication Use in Oncology (A Case Study in Glioblastoma). Front Pharmacol. 2019;10:681.
İyikesici MS, Slocum AK, Slocum A, Berkarda FB, Kalamian M, Seyfried TN: Efficacy of metabolically supported chemotherapy combined with ketogenic diet, hyperthermia, and hyperbaric oxygen therapy for stage IV triple-negative breast cancer. Cureus 2017, 9(7).
Jansen N, Walach H. The development of tumours under a ketogenic diet in association with the novel tumour marker TKTL1: a case series in general practice. Oncol Lett. 2016;11(1):584–92.
Medlinskiene K, Tomlinson J, Marques I, Richardson S, Stirling K, Petty D. Barriers and facilitators to the uptake of new medicines into clinical practice: a systematic review. BMC Health Serv Res. 2021;21(1):1198.
Veatch RM. Doctor does not know best: why in the new century physicians must stop trying to benefit patients. The Journal of medicine philosophy. 2000;25(6):701–21.
Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458–65.
Noakes TD, Kalamian M, Seyfried TN, Mukherjee P, D’Agostino DP, Arismendi-Morillo G, Chinopoulos C, Tettenborn M, Winters N: Cancer. In: Ketogenic. edn. Edited by Noakes TD, Murphy T, Wellington N, Kajee H, Rice SM: Academic Press; 2023: 307–362.
Wittich CM, Burkle CM, Lanier WL: Ten common questions (and their answers) about off-label drug use. In: Mayo Clin Proc: 2012: Elsevier; 2012: 982–990.
Borysowski J, Gorski A. Compassionate use of unauthorized drugs: Legal regulations and ethical challenges. Eur J Intern Med. 2019;65:12–6.
Fontanals S, Esteve A, Gonzalez A, Ibanez C, Martinez J, Mesia R, Clopes A. Real-world treatment outcomes of medicines used in special situations (off-label and compassionate use) in oncology and hematology: A retrospective study from a comprehensive cancer institution. Cancer Med. 2023;12(16):17112–25.
Krzyzanowska MK. Off-label use of cancer drugs: a benchmark is established. J Clin Oncol. 2013;31(9):1125–7.
Organization WH: Repurposing of medicines–the underrated champion of sustainable innovation: policy brief. In.: World Health Organization. Regional Office for Europe; 2021.
Lynch HF, Zettler PJ, Sarpatwari A. Promoting Patient Interests in Implementing the Federal Right to Try Act. JAMA. 2018;320(9):869–70.
Trojanowski P, Jarosz B, Szczepanek D. The diagnostic quality of needle brain biopsy specimens obtained with different sampling methods – Experimental study. Sci Rep. 2019;9(1):8077.
Alieva M, Margarido AS, Wieles T, Abels ER, Colak B, Boquetale C, Jan Noordmans H, Snijders TJ, Broekman ML, van Rheenen J. Preventing inflammation inhibits biopsy-mediated changes in tumor cell behavior. Sci Rep. 2017;7(1):7529.
Kameyama H, Dondapati P, Simmons R, Leslie M, Langenheim JF, Sun Y, Yi M, Rottschaefer A, Pathak R, Nuguri S, et al. Needle biopsy accelerates pro-metastatic changes and systemic dissemination in breast cancer: Implications for mortality by surgery delay. Cell Rep Med. 2023;4(12): 101330.
Noch EK, Sait SF, Farooq S, Trippett TM, Miller AM. A case series of extraneural metastatic glioblastoma at Memorial Sloan Kettering Cancer Center. Neurooncol Pract. 2021;8(3):325–36.
Ronvaux L, Riva M, Coosemans A, Herzog M, Rommelaere G, Donis N, D’Hondt L, Douxfils J. Liquid Biopsy in Glioblastoma Cancers (Basel). 2022;14(14):3394.
Gritsch S, Batchelor TT, Gonzalez Castro LN. Diagnostic, therapeutic, and prognostic implications of the 2021 World Health Organization classification of tumors of the central nervous system. Cancer. 2022;128(1):47–58.
Agarwal A, Edgar MA, Desai A, Gupta V, Soni N, Bathla G. Molecular GBM versus Histopathological GBM: Radiology-Pathology-Genetic Correlation and the New WHO 2021 Definition of Glioblastoma. AJNR Am J Neuroradiol. 2024;45(8):1006–12.
Costelloe CM, Amini B, Madewell JE: Risks and benefits of gadolinium-based contrast-enhanced MRI. In: Seminars in Ultrasound, CT and MRI: 2020: Elsevier; 2020: 170–182.
Brown SD. Professional norms regarding how radiologists handle incidental findings. J Am Coll Radiol. 2013;10(4):253–7.
Doubeni CA, Gabler NB, Wheeler CM, McCarthy AM, Castle PE, Halm EA, Schnall MD, Skinner CS, Tosteson ANA, Weaver DL, et al. Timely follow-up of positive cancer screening results: A systematic review and recommendations from the PROSPR Consortium. CA Cancer J Clin. 2018;68(3):199–216.
Lee TH, Brennan TA. Direct-to-consumer marketing of high-technology screening tests. N Engl J Med. 2002;346(7):529–31.
Hitzeman N, Cotton E. Incidentalomas: initial management. Am Fam Physician. 2014;90(11):784–9.
Aghi M, Barker Ii FG. Benign adult brain tumors: an evidence-based medicine review. Prog Neurol Surg. 2006;19:80–96.
Michelson N, Rincon-Torroella J, Quinones-Hinojosa A, Greenfield JP. Exploring the role of inflammation in the malignant transformation of low-grade gliomas. J Neuroimmunol. 2016;297:132–40.
Zhao H, Jin H, Xian J, Zhang Z, Shi J, Bai X. Effect of Ketogenic Diets on Body Composition and Metabolic Parameters of Cancer Patients: A Systematic Review and Meta-Analysis. Nutrients. 2022;14(19):4192.
Chaudhary R: Ketogenic Diet as a Treatment and Prevention Strategy for Cancer: A Therapeutic Alternative. Nutrition 2024:112427.
Mishra A, Giuliani G, Longo VD. Nutrition and dietary restrictions in cancer prevention. Biochim Biophys Acta Rev Cancer. 2024;1879(1): 189063.
Kwok KHF, Ip EC, Lee SF. The conundrums of the reasonable patient standard in English medical law. BMC Med Ethics. 2023;24(1):15.
Akeeb AA, King SM, Olaku O, White JD. Communication between cancer patients and physicians about complementary and alternative medicine: A systematic review. Journal of Integrative Complementary Medicine. 2023;29(2):80–98.
Rosenbaum L. The paternalism preference—choosing unshared decision making. Obstetrical Gynecological Survey. 2015;70(12):739–40.
Cherny NI, Sullivan R, Dafni U, Kerst JM, Sobrero A, Zielinski C, de Vries EG, Piccart MJ. A standardised, generic, validated approach to stratify the magnitude of clinical benefit that can be anticipated from anti-cancer therapies: the European Society for Medical Oncology Magnitude of Clinical Benefit Scale (ESMO-MCBS). Ann Oncol. 2015;26(8):1547–73.
Stahl D, Tomlinson T. Is there a right not to know? Nat Rev Clin Oncol. 2017;14(5):259–60.
Helgesson G. What is a reasonable framework for new non-validated treatments? Theoretical Medicine Bioethics. 2020;41:239–45.
Neal EG, Zupec-Kania B, Pfeifer HH. Carnitine, nutritional supplementation and discontinuation of ketogenic diet therapies. Epilepsy Res. 2012;100(3):267–71.
Elisia I, Krystal G. The Pros and Cons of Low Carbohydrate and Ketogenic Diets in the Prevention and Treatment of Cancer. Front Nutr. 2021;8: 634845.
Arvanitis CD, Ferraro GB, Jain RK. The blood-brain barrier and blood-tumour barrier in brain tumours and metastases. Nat Rev Cancer. 2020;20(1):26–41.
Pierscianek D, Ahmadipour Y, Oppong MD, Rauschenbach L, Kebir S, Glas M, Sure U, Jabbarli R. Blood-Based Biomarkers in High Grade Gliomas: a Systematic Review. Mol Neurobiol. 2019;56(9):6071–9.
Zachariah MA, Oliveira-Costa JP, Carter BS, Stott SL, Nahed BV. Blood-based biomarkers for the diagnosis and monitoring of gliomas. Neuro Oncol. 2018;20(9):1155–61.
Miller AM, Shah RH, Pentsova EI, Pourmaleki M, Briggs S, Distefano N, Zheng Y, Skakodub A, Mehta SA, Campos C, et al. Tracking tumour evolution in glioma through liquid biopsies of cerebrospinal fluid. Nature. 2019;565(7741):654–8.
Müller Bark J, Kulasinghe A, Chua B, Day BW, Punyadeera C. Circulating biomarkers in patients with glioblastoma. Br J Cancer. 2020;122(3):295–305.
Jelski W, Mroczko B. Molecular and Circulating Biomarkers of Brain Tumors. Int J Mol Sci. 2021;22(13):7039.
Cescon DW, Bratman SV, Chan SM, Siu LL. Circulating tumor DNA and liquid biopsy in oncology. Nat Cancer. 2020;1(3):276–90.
Hoffer OA, Ben-David MA, Katz E, Zoltnik Kirshenabum D, Alezra D, Zimmer Y, Kelson I, Gannot I. Thermal imaging as a tool for evaluating tumor treatment efficacy. J Biomed Opt. 2018;23(5):1–6.
Sadeghi-Naini A, Sannachi L, Tadayyon H, Tran WT, Slodkowska E, Trudeau M, Gandhi S, Pritchard K, Kolios MC, Czarnota GJ. Chemotherapy-Response Monitoring of Breast Cancer Patients Using Quantitative Ultrasound-Based Intra-Tumour Heterogeneities. Sci Rep. 2017;7(1):10352.
Zhang Y, Zhao J, Wang Y, Cai W, Zhang X, Li K, Liu W, Zhao Y, Kang H. Changes of Tumor Markers in Patients with Breast Cancer during Postoperative Adjuvant Chemotherapy. Dis Markers. 2022;2022:7739777.
Venniyoor A, Al Bahrani B, Rajan B. The Dilemma of Serum Tumor Marker (STM) Flares. Gulf J Oncolog. 2014;1(15):63–7.
Kurebayashi J, Nishimura R, Tanaka K, Kohno N, Kurosumi M, Moriya T, Ogawa Y, Taguchi T. Significance of serum tumor markers in monitoring advanced breast cancer patients treated with systemic therapy: a prospective study. Breast Cancer. 2004;11(4):389–95.
Kim HS, Park YH, Park MJ, Chang MH, Jun HJ, Kim KH, Ahn JS, Kang WK, Park K, Im YH. Clinical significance of a serum CA15-3 surge and the usefulness of CA15-3 kinetics in monitoring chemotherapy response in patients with metastatic breast cancer. Breast Cancer Res Treat. 2009;118(1):89–97.
Yasasever V, Dincer M, Camlica H, Karaloglu D, Dalay N. Utility of CA 15–3 and CEA in monitoring breast cancer patients with bone metastases: special emphasis on “spiking” phenomena. Clin Biochem. 1997;30(1):53–6.
Kim HJ, Lee KW, Kim YJ, Oh DY, Kim JH, Im SA, Lee JS. Chemotherapy-induced transient CEA and CA19-9 surges in patients with metastatic or recurrent gastric cancer. Acta Oncol. 2009;48(3):385–90.
Guadagni S, Masedu F, Fiorentini G, Sarti D, Fiorentini C, Guadagni V, Apostolou P, Papasotiriou I, Parsonidis P, Valenti M, et al. Circulating tumour cell gene expression and chemosensitivity analyses: predictive accuracy for response to multidisciplinary treatment of patients with unresectable refractory recurrent rectal cancer or unresectable refractory colorectal cancer liver metastases. BMC Cancer. 2022;22(1):660.
Anichini G, Fulmali P, O’Neill K, Datta V, Crook T, Syed N: PATH-24. ACCURATE IDENTIFICATION OF GLIAL MALIGNANCIES FROM PERIPHERAL BLOOD. Neuro Oncol 2022, 24(Supplement_7):vii155-vii155.
Valentini MC, Mellai M, Annovazzi L, Melcarne A, Denysenko T, Cassoni P, Casalone C, Maurella C, Grifoni S, Fania P, et al. Comparison among conventional and advanced MRI, (18)F-FDG PET/CT, phenotype and genotype in glioblastoma. Oncotarget. 2017;8(53):91636–53.
Venneti S, Dunphy MP, Zhang H, Pitter KL, Zanzonico P, Campos C, Carlin SD, La Rocca G, Lyashchenko S, Ploessl K et al: Glutamine-based PET imaging facilitates enhanced metabolic evaluation of gliomas in vivo. Sci Transl Med 2015, 7(274):274ra217.
Albert NL, Weller M, Suchorska B, Galldiks N, Soffietti R, Kim MM, la Fougere C, Pope W, Law I, Arbizu J, et al. Response Assessment in Neuro-Oncology working group and European Association for Neuro-Oncology recommendations for the clinical use of PET imaging in gliomas. Neuro Oncol. 2016;18(9):1199–208.
Galldiks N, Niyazi M, Grosu AL, Kocher M, Langen K-J, Law I, Minniti G, Kim MM, Tsien C, Dhermain F. Contribution of PET imaging to radiotherapy planning and monitoring in glioma patients-a report of the PET/RANO group. Neuro Oncol. 2021;23(6):881–93.
Okumura W, Iwasaki T, Toyama T, Iso T, Arai M, Oriuchi N, Endo K, Yokoyama T, Suzuki T, Kurabayashi M. Usefulness of fasting 18F-FDG PET in identification of cardiac sarcoidosis. J Nucl Med. 2004;45(12):1989–98.
Lee KH, Ko BH, Paik JY, Jung KH, Choe YS, Choi Y, Kim BT. Effects of anesthetic agents and fasting duration on 18F-FDG biodistribution and insulin levels in tumor-bearing mice. J Nucl Med. 2005;46(9):1531–6.
Bennett OA, Ramsay SC, Malacova E, Bourgeat P, Goodman SJ, Dunn CJ, Robinson BM, Lee K, Pattison DA. Regional differences in the reduction in cerebral FDG uptake induced by the ketogenic diet. Eur J Hybrid Imaging. 2022;6(1):29.
Doche E, Phlip M, Cammilleri S, Suissa L, GUEDJ E: Regional brain glucose metabolism is differentially affected by ketogenic diet: A human semiquantitative positron emission tomography. 2022.
Kim M, Eleftheriou A, Ravotto L, Weber B, Rivlin M, Navon G, Capozza M, Anemone A, Longo DL, Aime S. What do we know about dynamic glucose-enhanced (DGE) MRI and how close is it to the clinics? Horizon 2020 GLINT consortium report. Magnetic Resonance Materials in Physics, Biology Medicine. 2022;35(1):87–104.
Schmidt CA, Fisher-Wellman KH, Neufer PD. From OCR and ECAR to energy: Perspectives on the design and interpretation of bioenergetics studies. J Biol Chem. 2021;297(4): 101140.
Wang Y, Patti GJ. The Warburg effect: a signature of mitochondrial overload. Trends Cell Biol. 2023;33(12):1014–20.
Qian L, Li Y, Cao Y, Meng G, Peng J, Li H, Wang Y, Xu T, Zhang L, Sun B, et al. Pan-Cancer Analysis of Glycolytic and Ketone Bodies Metabolic Genes: Implications for Response to Ketogenic Dietary Therapy. Front Oncol. 2021;11: 689068.
Vallejo FA, Shah SS, de Cordoba N, Walters WM, Prince J, Khatib Z, Komotar RJ, Vanni S, Graham RM. The contribution of ketone bodies to glycolytic inhibition for the treatment of adult and pediatric glioblastoma. J Neurooncol. 2020;147:317–26.
Ludikhuize MC, Meerlo M, Burgering BMT, Rodriguez Colman MJ. Protocol to profile the bioenergetics of organoids using Seahorse. STAR Protoc. 2021;2(1): 100386.
Boykov I, Montgomery M, Hagen J, Aruleba R, McLaughlin K, Coalson H, Nelson M, Pereyra A, Ellis J, Zeczycki T et al: Pan-tissue mitochondrial phenotyping reveals lower OXPHOS expression and function across tumor types. 2023:2023.2006.2004.542600.
Sainero-Alcolado L, Liano-Pons J, Ruiz-Perez MV, Arsenian-Henriksson M. Targeting mitochondrial metabolism for precision medicine in cancer. Cell Death Differ. 2022;29(7):1304–17.
Butler M, van der Meer LT, van Leeuwen FN. Amino Acid Depletion Therapies: Starving Cancer Cells to Death. Trends Endocrinol Metab. 2021;32(6):367–81.
Lee H, Woo SM, Jang H, Kang M, Kim S-Y: Cancer depends on fatty acids for ATP production: A possible link between cancer and obesity. In: Seminars in Cancer Biology: 2022: Elsevier; 2022.
Ying M, You D, Zhu X, Cai L, Zeng S, Hu X. Lactate and glutamine support NADPH generation in cancer cells under glucose deprived conditions. Redox Biol. 2021;46: 102065.
Zhang X, Dang CV. Time to hit pause on mitochondria-targeting cancer therapies. Nat Med. 2023;29(1):29–30.
Wang ZH, Chen L, Li W, Chen L, Wang YP. Mitochondria transfer and transplantation in human health and diseases. Mitochondrion. 2022;65:80–7.
Zhou W, Zhao Z, Yu Z, Hou Y, Keerthiga R, Fu A. Mitochondrial transplantation therapy inhibits the proliferation of malignant hepatocellular carcinoma and its mechanism. Mitochondrion. 2022;65:11–22.
Chang JC, Chang HS, Wu YC, Cheng WL, Lin TT, Chang HJ, Kuo SJ, Chen ST, Liu CS. Mitochondrial transplantation regulates antitumour activity, chemoresistance and mitochondrial dynamics in breast cancer. J Exp Clin Cancer Res. 2019;38(1):30.
Koh S, Dupuis N, Auvin S. Ketogenic diet and Neuroinflammation. Epilepsy Res. 2020;167: 106454.
Han C. Potential Value of Positron Emission Tomography (PET) in Evaluating the Ketogenic Diet as Anticancer Therapy. Journal of Nutritional Oncology. 2018;3(2):49–54.
Cussó L, Musteanu M, Mulero F, Barbacid M, Desco M. Effects of a ketogenic diet on [18 F] FDG-PET imaging in a mouse model of lung cancer. Mol Imag Biol. 2019;21:279–85.
Martin-McGill KJ, Marson AG, Tudur Smith C, Jenkinson MD. Ketogenic diets as an adjuvant therapy in glioblastoma (the KEATING trial): study protocol for a randomised pilot study. Pilot feasibility studies. 2017;3:1–11.
Stummer W. Extent of resection and survival in glioblastoma multiforme. Neurosurgery. 2009;64(6):E1206.
Baig Mirza A, Christodoulides I, Lavrador JP, Giamouriadis A, Vastani A, Boardman T, Ahmed R, Norman I, Murphy C, Devi S. 5-Aminolevulinic acid-guided resection improves the overall survival of patients with glioblastoma—A comparative cohort study of 343 patients. Neuro-oncology advances. 2021;3(1):vdab047.
Voskuil FJ, Steinkamp PJ, Zhao T, van der Vegt B, Koller M, Doff JJ, Jayalakshmi Y, Hartung JP, Gao J, Sumer BD, et al. Exploiting metabolic acidosis in solid cancers using a tumor-agnostic pH-activatable nanoprobe for fluorescence-guided surgery. Nat Commun. 2020;11(1):3257.
Netufo O, Connor K, Shiels LP, Sweeney KJ, Wu D, O’Shea DF, Byrne AT, Miller IS. Refining Glioblastoma Surgery through the Use of Intra-Operative Fluorescence Imaging Agents. Pharmaceuticals (Basel). 2022;15(5):550.
Barbagallo GM, Jenkinson MD, Brodbelt AR. ‘Recurrent’glioblastoma multiforme, when should we reoperate? Br J Neurosurg. 2008;22(3):452–5.
De Bonis P, Anile C, Pompucci A, Fiorentino A, Balducci M, Chiesa S, Lauriola L, Maira G, Mangiola A. The influence of surgery on recurrence pattern of glioblastoma. Clin Neurol Neurosurg. 2013;115(1):37–43.
Dejaegher J, De Vleeschouwer S: Recurring glioblastoma: A case for reoperation? Exon Publications 2017:281–296.
Germano IM, Johnson DR, Patrick HH, Goodman AL, Ziu M, Ormond DR, Olson JJ. Congress of Neurological Surgeons Systematic Review and Evidence-Based Guidelines on the Management of Progressive Glioblastoma in Adults: Update of the 2014 Guidelines. Neurosurgery. 2022;90(5):e112–5.
Valencia I, Pfeifer H, Thiele EA. General anesthesia and the ketogenic diet: clinical experience in nine patients. Epilepsia. 2002;43(5):525–9.
Albanese A, Prevedello L, Markovich M, Busetto L, Vettor R, Foletto M: Pre-operative Very Low Calorie Ketogenic Diet (VLCKD) vs. Very Low Calorie Diet (VLCD): Surgical Impact. Obes Surg 2019, 29(1):292–296.
Forsythe CE, Phinney SD, Fernandez ML, Quann EE, Wood RJ, Bibus DM, Kraemer WJ, Feinman RD, Volek JS. Comparison of low fat and low carbohydrate diets on circulating fatty acid composition and markers of inflammation. Lipids. 2008;43(1):65–77.
Jordan S, Tung N, Casanova-Acebes M, Chang C, Cantoni C, Zhang D, Wirtz TH, Naik S, Rose SA, Brocker CN et al: Dietary Intake Regulates the Circulating Inflammatory Monocyte Pool. Cell 2019, 178(5):1102–1114 e1117.
Abd Ellatif RA, Ibrahim MA: Ketogenic diet enhances delayed wound healing in immunocompromised rats: A histological and immunohistochemical study. Egyptian Journal of Histology 2021.
Kesl S, Jung M, Prather J, Sherwood J, Gould L, D’Agostino D: Sustaining dietary ketosis to improve blood flow and wound healing in young and aged Fisher rats (734.7). The FASEB Journal 2014, 28:734.737.
Lu Y, Yang Y-Y, Zhou M-W, Liu N, Xing H-Y, Liu X-X, Li F. Ketogenic diet attenuates oxidative stress and inflammation after spinal cord injury by activating Nrf2 and suppressing the NF-κB signaling pathways. Neurosci Lett. 2018;683:13–8.
Sayadi JJ, Sayadi L, Satteson E, Chopan M. Nerve injury and repair in a ketogenic milieu: A systematic review of traumatic injuries to the spinal cord and peripheral nervous tissue. PLoS ONE. 2021;16(1): e0244244.
Masino SA, Ruskin DN. Ketogenic diets and pain. J Child Neurol. 2013;28(8):993–1001.
Włodarczyk A, Cubała WJ, Stawicki M. Ketogenic diet for depression: A potential dietary regimen to maintain euthymia? Progress in Neuro-Psychopharmacology Biological Psychiatry. 2021;109: 110257.
Lussier DM, Woolf EC, Johnson JL, Brooks KS, Blattman JN, Scheck AC. Enhanced immunity in a mouse model of malignant glioma is mediated by a therapeutic ketogenic diet. BMC Cancer. 2016;16(1):1–10.
Gomez-Arbelaez D, Bellido D, Castro AI, Ordonez-Mayan L, Carreira J, Galban C, Martinez-Olmos MA, Crujeiras AB, Sajoux I, Casanueva FF. Body Composition Changes After Very-Low-Calorie Ketogenic Diet in Obesity Evaluated by 3 Standardized Methods. J Clin Endocrinol Metab. 2017;102(2):488–98.
Masood W, Annamaraju P, Uppaluri KR: Ketogenic diet. In: StatPearls. edn.: StatPearls Publishing; 2021.
James LJ, Shirreffs SM. Effect of electrolyte addition to rehydration drinks consumed after severe fluid and energy restriction. J Strength Cond Res. 2015;29(2):521–7.
Watanabe M, Tozzi R, Risi R, Tuccinardi D, Mariani S, Basciani S, Spera G, Lubrano C, Gnessi L. Beneficial effects of the ketogenic diet on nonalcoholic fatty liver disease: A comprehensive review of the literature. Obes Rev. 2020;21(8): e13024.
Pietzner M, Uluvar B, Kolnes KJ, Jeppesen PB, Frivold SV, Skattebo O, Johansen EI, Skalhegg BS, Wojtaszewski JFP, Kolnes AJ, et al. Systemic proteome adaptions to 7-day complete caloric restriction in humans. Nat Metab. 2024;6(4):764–77.
Alirezaei M, Kemball CC, Flynn CT, Wood MR, Whitton JL, Kiosses WB. Short-term fasting induces profound neuronal autophagy. Autophagy. 2010;6(6):702–10.
Longo VD, Mattson MP. Fasting: molecular mechanisms and clinical applications. Cell Metab. 2014;19(2):181–92.
Ibrahim EM, Al-Foheidi MH, Al-Mansour MM. Energy and caloric restriction, and fasting and cancer: a narrative review. Support Care Cancer. 2021;29(5):2299–304.
Kikomeko J, Schutte T, van Velzen MJM, Seefat R, van Laarhoven HWM. Short-term fasting and fasting mimicking diets combined with chemotherapy: a narrative review. Ther Adv Med Oncol. 2023;15:17588359231161418.
de Groot S, Pijl H, van der Hoeven JJM, Kroep JR. Effects of short-term fasting on cancer treatment. J Exp Clin Cancer Res. 2019;38(1):209.
Wilhelmi de Toledo F, Buchinger A, Burggrabe H, Holz G, Kuhn C, Lischka E, Lischka N, Lutzner H, May W, Ritzmann-Widderich M et al: Fasting therapy – an expert panel update of the 2002 consensus guidelines. Forsch Komplementmed 2013, 20(6):434–443.
Nishimuta M, Kodama N, Yoshitake Y, Shimada M, Serizawa N. Dietary Salt (Sodium Chloride) Requirement and Adverse Effects of Salt Restriction in Humans. J Nutr Sci Vitaminol. 2018;64(2):83–9.
Garg R, Williams GH, Hurwitz S, Brown NJ, Hopkins PN, Adler GK. Low-salt diet increases insulin resistance in healthy subjects. Metabolism. 2011;60(7):965–8.
Lloyd-Mostyn RH, Lord PS, Glover R, West C, Gilliland IC. Uric acid metabolism in starvation. Ann Rheum Dis. 1970;29(5):553–5.
Teruya T, Chaleckis R, Takada J, Yanagida M, Kondoh H. Diverse metabolic reactions activated during 58-hr fasting are revealed by non-targeted metabolomic analysis of human blood. Sci Rep. 2019;9(1):854.
Gohari S, Ghobadi S, Jafari A, Ahangar H, Gohari S, Mahjani M. The effect of dietary approaches to stop hypertension and ketogenic diets intervention on serum uric acid concentration: a systematic review and meta-analysis of randomized controlled trials. Sci Rep. 2023;13(1):10492.
Anton SD, Moehl K, Donahoo WT, Marosi K, Lee SA, Mainous AG 3rd, Leeuwenburgh C, Mattson MP. Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting. Obesity (Silver Spring). 2018;26(2):254–68.
Hall KD, Chen KY, Guo J, Lam YY, Leibel RL, Mayer LE, Reitman ML, Rosenbaum M, Smith SR, Walsh BT, et al. Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men. Am J Clin Nutr. 2016;104(2):324–33.
Zupec-Kania BA, Aldaz V, Montgomery ME, Kostas KC: Enteral and parenteral applications of ketogenic diet therapy: experiences from four centers. ICAN: Infant, Child, Adolescent Nutrition 2011, 3(5):274–281.
Kaul N, Nation J, Laing J, Nicolo JP, Deane AM, Udy AA, Kwan P, O’Brien TJ. Modified low ratio ketogenic therapy in the treatment of adults with super-refractory status epilepticus. JPEN J Parenter Enteral Nutr. 2022;46(8):1819–27.
van der Louw E, Aldaz V, Harvey J, Roan M, van den Hurk D, Cross JH, Auvin S, Review G. Optimal clinical management of children receiving ketogenic parenteral nutrition: a clinical practice guide. Dev Med Child Neurol. 2020;62(1):48–56.
Walker MD, Strike TA, Sheline GE. An analysis of dose-effect relationship in the radiotherapy of malignant gliomas. Int J Radiat Oncol Biol Phys. 1979;5(10):1725–31.
Gzell C, Back M, Wheeler H, Bailey D, Foote M. Radiotherapy in Glioblastoma: the Past, the Present and the Future. Clin Oncol (R Coll Radiol). 2017;29(1):15–25.
Haggiagi A, Lassman AB: Newly diagnosed glioblastoma in the elderly: when is temozolomide alone enough? In., vol. 22: Oxford University Press US; 2020: 1058–1059.
Wick A, Kessler T, Platten M, Meisner C, Bamberg M, Herrlinger U, Felsberg J, Weyerbrock A, Papsdorf K, Steinbach JP, et al. Superiority of temozolomide over radiotherapy for elderly patients with RTK II methylation class, MGMT promoter methylated malignant astrocytoma. Neuro Oncol. 2020;22(8):1162–72.
Gupta K, Vuckovic I, Zhang S, Xiong Y, Carlson BL, Jacobs J, Olson I, Petterson XM, Macura SI, Sarkaria J, et al. Radiation Induced Metabolic Alterations Associate With Tumor Aggressiveness and Poor Outcome in Glioblastoma. Front Oncol. 2020;10:535.
Tabatabaei P, Visse E, Bergstrom P, Brannstrom T, Siesjo P, Bergenheim AT. Radiotherapy induces an immediate inflammatory reaction in malignant glioma: a clinical microdialysis study. J Neurooncol. 2017;131(1):83–92.
Arnold KM, Flynn NJ, Raben A, Romak L, Yu Y, Dicker AP, Mourtada F, Sims-Mourtada J. The Impact of Radiation on the Tumor Microenvironment: Effect of Dose and Fractionation Schedules. Cancer Growth Metastasis. 2018;11:1179064418761639.
Sundahl N, Duprez F, Ost P, De Neve W, Mareel M. Effects of radiation on the metastatic process. Mol Med. 2018;24(1):16.
Duan C, Yang R, Yuan L, Engelbach JA, Tsien CI, Rich KM, Dahiya SM, Johanns TM, Ackerman JJH, Garbow JR. Late Effects of Radiation Prime the Brain Microenvironment for Accelerated Tumor Growth. Int J Radiat Oncol Biol Phys. 2019;103(1):190–4.
Shankar A, Kumar S, Iskander AS, Varma NR, Janic B, deCarvalho A, Mikkelsen T, Frank JA, Ali MM, Knight RA, et al. Subcurative radiation significantly increases cell proliferation, invasion, and migration of primary glioblastoma multiforme in vivo. Chin J Cancer. 2014;33(3):148–58.
Gupta K, Burns TC. Radiation-Induced Alterations in the Recurrent Glioblastoma Microenvironment: Therapeutic Implications. Front Oncol. 2018;8:503.
Betlazar C, Middleton RJ, Banati RB, Liu GJ. The impact of high and low dose ionising radiation on the central nervous system. Redox Biol. 2016;9:144–56.
Cuccurullo V, Di Stasio GD, Cascini GL, Gatta G, Bianco C. The Molecular Effects of Ionizing Radiations on Brain Cells: Radiation Necrosis vs. Tumor Recurrence Diagnostics (Basel). 2019;9(4):127.
Carr CM, Benson JC, DeLone DR, Diehn FE, Kim DK, Merrell KW, Nagelschneider AA, Madhavan AA, Johnson DR. Intracranial long-term complications of radiation therapy: an image-based review. Neuroradiology. 2021;63(4):471–82.
Makale MT, McDonald CR, Hattangadi-Gluth JA, Kesari S. Mechanisms of radiotherapy-associated cognitive disability in patients with brain tumours. Nat Rev. 2017;13(1):52–64.
Kazda T, Dziacky A, Burkon P, Pospisil P, Slavik M, Rehak Z, Jancalek R, Slampa P, Slaby O, Lakomy R. Radiotherapy of glioblastoma 15 years after the landmark Stupp’s trial: more controversies than standards? Radiology oncology. 2018;52(2):121–8.
Ziu M, Kim BYS, Jiang W, Ryken T, Olson JJ. The role of radiation therapy in treatment of adults with newly diagnosed glioblastoma multiforme: a systematic review and evidence-based clinical practice guideline update. J Neurooncol. 2020;150(2):215–67.
Colangelo NW, Azzam EI. Extracellular vesicles originating from glioblastoma cells increase metalloproteinase release by astrocytes: the role of CD147 (EMMPRIN) and ionizing radiation. Cell Commun Signal. 2020;18(1):21.
Lawrie TA, Gillespie D, Dowswell T, Evans J, Erridge S, Vale L, Kernohan A, Grant R. Long-term neurocognitive and other side effects of radiotherapy, with or without chemotherapy, for glioma. Cochrane Database Syst Rev. 2019;8(8):CD013047.
Guram K, Smith M, Ginader T, Bodeker K, Pelland D, Pennington E, Buatti JM. Using smaller-than-standard radiation treatment margins does not change survival outcomes in patients with high-grade gliomas. Pract Radiat Oncol. 2019;9(1):16–23.
Zeng Q, Stylianou T, Preston J, Glover S, O’Neill K, Woolf EC, Scheck AC, Syed N: The ketogenic diet alters the epigenetic landscape of GBM to potentiate the effects of chemotherapy and radiotherapy. Neuro Oncol 2019, 21(Supplement_4):iv8-iv8.
Abdelwahab MG, Fenton KE, Preul MC, Rho JM, Lynch A, Stafford P, Scheck AC. The ketogenic diet is an effective adjuvant to radiation therapy for the treatment of malignant glioma. PLoS ONE. 2012;7(5): e36197.
Balducci M, Chiesa S, Diletto B, D’Agostino GR, Mangiola A, Manfrida S, Mantini G, Albanese A, Fiorentino A, Frascino V, et al. Low-dose fractionated radiotherapy and concomitant chemotherapy in glioblastoma multiforme with poor prognosis: a feasibility study. Neuro Oncol. 2012;14(1):79–86.
Bergman D, Modh A, Schultz L, Snyder J, Mikkelsen T, Shah M, Ryu S, Siddiqui MS, Walbert T. Randomized prospective trial of fractionated stereotactic radiosurgery with chemotherapy versus chemotherapy alone for bevacizumab-resistant high-grade glioma. J Neurooncol. 2020;148(2):353–61.
Klement RJ. The influence of ketogenic therapy on the 5 R’s of radiobiology. Int J Radiat Biol. 2019;95(4):394–407.
Valayer S, Kim D, Fogtman A, Straube U, Winnard A, Caplan N, Green DA, van Leeuwen FHP, Weber T. The Potential of Fasting and Caloric Restriction to Mitigate Radiation Damage-A Systematic Review. Front Nutr. 2020;7: 584543.
Icard P, Ollivier L, Forgez P, Otz J, Alifano M, Fournel L, Loi M, Thariat J. Perspective: Do fasting, caloric restriction, and diets increase sensitivity to radiotherapy? A literature review. Adv Nutr. 2020;11(5):1089–101.
Beauchamp T, Childress J. Principles of Biomedical Ethics: Marking Its Fortieth Anniversary. Am J Bioeth. 2019;19(11):9–12.
Association WM. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4.
Matsuyama R, Reddy S, Smith TJ. Why do patients choose chemotherapy near the end of life? A review of the perspective of those facing death from cancer. J Clin Oncol. 2006;24(21):3490–6.
Winter SF, Vaios EJ, Shih HA, Grassberger C, Parsons MW, Gardner MM, Ehret F, Kaul D, Boehmerle W, Endres M, et al. Mitigating Radiotoxicity in the Central Nervous System: Role of Proton Therapy. Curr Treat Options Oncol. 2023;24(11):1524–49.
Giles AJ, Hutchinson MND, Sonnemann HM, Jung J, Fecci PE, Ratnam NM, Zhang W, Song H, Bailey R, Davis D, et al. Dexamethasone-induced immunosuppression: mechanisms and implications for immunotherapy. J Immunother Cancer. 2018;6(1):51.
Stokum JA, Gerzanich V, Sheth KN, Kimberly WT, Simard JM. Emerging Pharmacological Treatments for Cerebral Edema: Evidence from Clinical Studies. Annu Rev Pharmacol Toxicol. 2020;60:291–309.
Carpentier AF, Ferrari D, Bailon O, Ursu R, Banissi C, Dubessy AL, Belin C, Levy C. Steroid-sparing effects of angiotensin-II inhibitors in glioblastoma patients. Eur J Neurol. 2012;19(10):1337–42.
Goldman M, Lucke-Wold B, Martinez-Sosa M, Katz J, Mehkri Y, Valisno J, Quintin S. Steroid utility, immunotherapy, and brain tumor management: an update on conflicting therapies. Explor Target Antitumor Ther. 2022;3(5):659–75.
Rangwala BS, Shakil A, Mustafa MS, Rangwala HS, Fatima H, Siddiq MA. Losartan and Immune Checkpoint Inhibitors in Glioblastoma: An Appropriate Substitute for Steroids. Ann Neurosci. 2024;31(3):152–4.
Kirste S, Treier M, Wehrle SJ, Becker G, Abdel-Tawab M, Gerbeth K, Hug MJ, Lubrich B, Grosu AL, Momm F. Boswellia serrata acts on cerebral edema in patients irradiated for brain tumors: a prospective, randomized, placebo-controlled, double-blind pilot trial. Cancer. 2011;117(16):3788–95.
Dubinski D, Hattingen E, Senft C, Seifert V, Peters KG, Reiss Y, Devraj K, Plate KH. Controversial roles for dexamethasone in glioblastoma – Opportunities for novel vascular targeting therapies. J Cereb Blood Flow Metab. 2019;39(8):1460–8.
Lim-Fat MJ, Bi WL, Lo J, Lee EQ, Ahluwalia MS, Batchelor TT, Chang SM, Chiocca EA, Chukwueke U, Cloughesy TF, et al. Letter: When Less is More: Dexamethasone Dosing for Brain Tumors. Neurosurgery. 2019;85(3):E607–8.
Amaral L, Gresham G, Kim S, Tighiouart M, Nelson T, Welborn A, Lockshon L, Noorvash B, Rudnick JD, Irwin SA. The ketogenic diet plus standard of care for adults with recently diagnosed glioblastoma: Results from a phase 1 trial. In.: American Society of Clinical Oncology; 2023.
Klement RJ. The emerging role of ketogenic diets in cancer treatment. Curr Opin Clin Nutr Metab Care. 2019;22(2):129–34.
Soeters MR, Soeters PB, Schooneman MG, Houten SM, Romijn JA. Adaptive reciprocity of lipid and glucose metabolism in human short-term starvation. Am J Physiol. 2012;303(12):E1397–1407.
Reinfeld BI, Madden MZ, Wolf MM, Chytil A, Bader JE, Patterson AR, Sugiura A, Cohen AS, Ali A, Do BT, et al. Cell-programmed nutrient partitioning in the tumour microenvironment. Nature. 2021;593(7858):282–8.
Cohen AS, Grudzinski J, Smith GT, Peterson TE, Whisenant JG, Hickman TL, Ciombor KK, Cardin D, Eng C, Goff LW, et al. First-in-Human PET Imaging and Estimated Radiation Dosimetry of l-[5-(11)C]-Glutamine in Patients with Metastatic Colorectal Cancer. J Nucl Med. 2022;63(1):36–43.
Alomari S, Zhang I, Hernandez A, Kraft CY, Raj D, Kedda J, Tyler B. Drug Repurposing for Glioblastoma and Current Advances in Drug Delivery-A Comprehensive Review of the Literature. Biomolecules. 2021;11(12):1870.
Basso J, Miranda A, Sousa J, Pais A, Vitorino C. Repurposing drugs for glioblastoma: From bench to bedside. Cancer Lett. 2018;428:173–83.
Serafin MB, Bottega A, da Rosa TF, Machado CS, Foletto VS, Coelho SS, da Mota AD, Horner R. Drug Repositioning in Oncology. Am J Ther. 2021;28(1):e111–7.
Harrison RK. Phase II and phase III failures: 2013–2015. Nat Rev Drug Discov. 2016;15(12):817–8.
Ranganathan S, Haslam A, Tuia J, Prasad V. Characteristics and outcomes of new molecular oncology drug approvals, in combination or monotherapy. J Cancer Policy. 2024;39: 100462.
Hall PE, Lewis R, Syed N, Shaffer R, Evanson J, Ellis S, Williams M, Feng X, Johnston A, Thomson JA, et al. A Phase I Study of Pegylated Arginine Deiminase (Pegargiminase), Cisplatin, and Pemetrexed in Argininosuccinate Synthetase 1-Deficient Recurrent High-grade Glioma. Clin Cancer Res. 2019;25(9):2708–16.
Breckenridge A, Jacob R. Overcoming the legal and regulatory barriers to drug repurposing. Nat Rev Drug Discov. 2019;18(1):1–2.
Oprea TI, Mestres J. Drug repurposing: far beyond new targets for old drugs. AAPS J. 2012;14(4):759–63.
Cha GD, Jung S, Choi SH, Kim DH. Local Drug Delivery Strategies for Glioblastoma Treatment. Brain Tumor Res Treat. 2022;10(3):151–7.
Verbaanderd C, Rooman I, Meheus L, Huys I. On-Label or Off-Label? Overcoming Regulatory and Financial Barriers to Bring Repurposed Medicines to Cancer Patients. Front Pharmacol. 2019;10:1664.
Zhang Y, Li Q, Huang Z, Li B, Nice EC, Huang C, Wei L, Zou B. Targeting glucose metabolism enzymes in cancer treatment: current and emerging strategies. Cancers (Basel). 2022;14(19):4568.
Fiveash JB, Ye X, Peerboom DM, Mikkelsen T, Chowdhary S, Rosenfeld M, Lesser GJ, Fisher J, Desideri S, Grossman S, et al. Clinical trials of R-(-)-gossypol (AT-101) in newly diagnosed and recurrent glioblastoma: NABTT 0602 and NABTT 0702. PLoS ONE. 2024;19(1): e0291128.
Wang Z, Liu F, Fan N, Zhou C, Li D, Macvicar T, Dong Q, Bruns CJ, Zhao Y. Targeting Glutaminolysis: New Perspectives to Understand Cancer Development and Novel Strategies for Potential Target Therapies. Front Oncol. 2020;10: 589508.
Yap TA, Dumbrava EE, Rodon Ahnert J, Hong DS, Pant S, Karp DD, Piha-Paul SAA, Subbiah V, Tsimberidou AM, Fu S: First-in-human biomarker-driven phase I trial of the potent and selective glutaminase-1 (GLS1) inhibitor IACS-6274 (IPN60090) in patients (pts) with molecularly selected advanced solid tumors. In.: Wolters Kluwer Health; 2021.
DeBerardinis RJ. Tumor Microenvironment, Metabolism, and Immunotherapy. N Engl J Med. 2020;382(9):869–71.
Bhatia K. Bhumika, Das A: Combinatorial drug therapy in cancer – New insights. Life Sci. 2020;258: 118134.
Ngoi NYL, Eu JQ, Hirpara J, Wang L, Lim JSJ, Lee SC, Lim YC, Pervaiz S, Goh BC, Wong ALA. Targeting Cell Metabolism as Cancer Therapy. Antioxid Redox Signal. 2020;32(5):285–308.
Takhwifa F, Aninditha T, Setiawan H, Sauriasari R. The potential of metformin as an antineoplastic in brain tumors: A systematic review. Heliyon. 2021;7(4): e06558.
Wang S, Lin Y, Xiong X, Wang L, Guo Y, Chen Y, Chen S, Wang G, Lin P, Chen H. Low-Dose Metformin Reprograms the Tumor Immune Microenvironment in Human Esophageal Cancer: Results of a Phase II Clinical TrialLow-Dose Metformin Turns TIME against Cancer. Clin Cancer Res. 2020;26(18):4921–32.
Kim HS, Kim JH, Jang HJ, Lee J. The addition of metformin to systemic anticancer therapy in advanced or metastatic cancers: a meta-analysis of randomized controlled trials. Int J Med Sci. 2020;17(16):2551–60.
Fuentes-Fayos AC, ME GG, Perez-Gomez JM, Montero-Hidalgo AJ, Martin-Colom J, Doval-Rosa C, Blanco-Acevedo C, Torres E, Toledano-Delgado A, Sanchez-Sanchez R et al: Metformin and simvastatin exert additive antitumour effects in glioblastoma via senescence-state: clinical and translational evidence. EBioMedicine 2023, 90:104484.
Xie W, Su F, Wang G, Peng Z, Xu Y, Zhang Y, Xu N, Hou K, Hu Z, Chen Y, et al. Glucose-lowering effect of berberine on type 2 diabetes: A systematic review and meta-analysis. Front Pharmacol. 2022;13:1015045.
Jiang W, Finniss S, Cazacu S, Xiang C, Brodie Z, Mikkelsen T, Poisson L, Shackelford DB, Brodie C. Repurposing phenformin for the targeting of glioma stem cells and the treatment of glioblastoma. Oncotarget. 2016;7(35):56456–70.
Yendapally R, Sikazwe D, Kim SS, Ramsinghani S, Fraser-Spears R, Witte AP, La-Viola B. A review of phenformin, metformin, and imeglimin. Drug Dev Res. 2020;81(4):390–401.
Yap TA, Daver N, Mahendra M, Zhang J, Kamiya-Matsuoka C, Meric-Bernstam F, Kantarjian HM, Ravandi F, Collins ME, Francesco MED, et al. Complex I inhibitor of oxidative phosphorylation in advanced solid tumors and acute myeloid leukemia: phase I trials. Nat Med. 2023;29(1):115–26.
Machado ND, Heather LC, Harris AL, Higgins GS. Targeting mitochondrial oxidative phosphorylation: lessons, advantages, and opportunities. Br J Cancer. 2023;129(6):897–9.
Lau KTK, Ng L, Wong JWH, Loong HHF, Chan WWL, Lee CH, Wong CKH. Repurposing sodium-glucose co-transporter 2 inhibitors (SGLT2i) for cancer treatment – A Review. Rev Endocr Metab Disord. 2021;22(4):1121–36.
Park LK, Lim KH, Volkman J, Abdiannia M, Johnston H, Nigogosyan Z, Siegel MJ, McGill JB, McKee AM, Salam M, et al. Safety, tolerability, and effectiveness of the sodium-glucose cotransporter 2 inhibitor (SGLT2i) dapagliflozin in combination with standard chemotherapy for patients with advanced, inoperable pancreatic adenocarcinoma: a phase 1b observational study. Cancer Metab. 2023;11(1):6.
Luo J, Hendryx M, Dong Y. Sodium-glucose cotransporter 2 (SGLT2) inhibitors and non-small cell lung cancer survival. Br J Cancer. 2023;128(8):1541–7.
Kapila V, Topf J. Sodium-Glucose Co-transporter 2 Inhibitor-Associated Euglycemic Diabetic Ketoacidosis After Bariatric Surgery: A Case and Literature Review. Cureus. 2021;13(8): e17093.
Hendrickson AL, Ye XQ, Kalra SS, Franck AJ, Urbine D. Euglycemic Diabetic Ketoacidosis in a Patient Prescribed Empagliflozin and a Ketogenic Diet: A Case of Misdiagnosed Type 1 Diabetes. Clin Diabetes. 2021;39(1):121–3.
Dorcely B, Nitis J, Schwartzbard A, Newman JD, Goldberg IJ, Sum M. A Case Report: Euglycemic Diabetic Ketoacidosis Presenting as Chest Pain in a Patient on a Low Carbohydrate Diet. Curr Diabetes Rev. 2021;17(2):243–6.
Guirguis H, Beroukhim Afrahimi S, Pham C. The Use of SGLT-2 Inhibitors Coupled With a Strict Low-Carbohydrate Diet: A Set-Up for Inducing Severe Diabetic Ketoacidosis. Clin Med Insights Case Rep. 2022;15:11795476221090044.
Liu D, Weintraub MA, Garcia C, Goncalves MD, Sisk AE, Casas A, Harding JJ, Harnicar S, Drilon A, Jhaveri K, et al. Characterization, management, and risk factors of hyperglycemia during PI3K or AKT inhibitor treatment. Cancer Med. 2022;11(8):1796–804.
Senior M. Precision nutrition to boost cancer treatments. Nat Biotechnol. 2022;40(10):1422–4.
Sissung TM, Schmidt KT, Figg WD. Insulin potentiation therapy for cancer? Lancet Oncol. 2019;20(2):191–2.
Poff AM, Moss S, Soliven M, D’Agostino DP. Ketone Supplementation: Meeting the Needs of the Brain in an Energy Crisis. Front Nutr. 2021;8: 783659.
Pajak B, Siwiak E, Soltyka M, Priebe A, Zielinski R, Fokt I, Ziemniak M, Jaskiewicz A, Borowski R, Domoradzki T, et al. 2-Deoxy-d-Glucose and Its Analogs: From Diagnostic to Therapeutic Agents. Int J Mol Sci. 2019;21(1):234.
Patil N, Howe O, Cahill P, Byrne HJ. Monitoring and modelling the dynamics of the cellular glycolysis pathway: A review and future perspectives. Mol Metab. 2022;66: 101635.
Becker AP, Sells BE, Haque SJ, Chakravarti A. Tumor Heterogeneity in Glioblastomas: From Light Microscopy to Molecular Pathology. Cancers (Basel). 2021;13(4):761.
Yuan S, Almagro J, Fuchs E. Beyond genetics: driving cancer with the tumour microenvironment behind the wheel. Nat Rev Cancer. 2024;24(4):274–86.
Pittillo R, Hunt D: Azaserine and 6-diazo-5-oxo-L-norleucine (DON). In: Antibiotics: Volume I Mechanism of Action. edn.: Springer; 1967: 481–493.
Lemberg KM, Vornov JJ, Rais R, Slusher BS. We’re not “DON” yet: optimal dosing and prodrug delivery of 6-Diazo-5-oxo-L-norleucine. Mol Cancer Ther. 2018;17(9):1824–32.
Rais R, Lemberg KM, Tenora L, Arwood ML, Pal A, Alt J, Wu Y, Lam J, Aguilar JMH, Zhao L et al: Discovery of DRP-104, a tumor-targeted metabolic inhibitor prodrug. Sci Adv 2022, 8(46):eabq5925.
Xu H, Zheng M, Yang C, Wang K, Lv Z, Liu Z, Tang Z, Chen X. Azo-based hypoxic-activated 6-diazo-5-oxo-L-norleucine (DON) prodrug combined with vascular disrupting agent nanoparticles for tumor-selective glutamine metabolism blockade. Chem Eng J. 2024;481: 148281.
Sklaroff RB, Casper ES, Magill GB, Young CW. Phase I study of 6-diazo-5-oxo-L-norleucine (DON). Cancer Treat Rep. 1980;64(12):1247–51.
Unger C, Müller C, Jäger E, Bausch M, Roberts J, Al-Batran S, Sethuraman N: Results from a phase I dose escalation study of PEGylated glutaminase in combination with 6-diazo-5-oxo-L-norleucine (DON) in advanced malignant solid tumors. Journal of Clinical Oncology 2006, 24(18_suppl):13017–13017.
Nampota-Nkomba N, Nyirenda OM, Mallewa J, Chimalizeni Y, Dzabala N, Fay MP, Gopalakrishnan M, Laurens MB, O’Brien NF, Miller LH, et al. DON in pediatric cerebral malaria, a phase I/IIA dose-escalation safety study: study protocol for a clinical trial. Trials. 2024;25(1):87.
Magill G, Myers W, Reilly H, Putnam R, Magill J, Sykes M, Escher G, Karnofsky D, Burchenal J. Pharmacological and initial therapeutic observations on 6-Diazo-5-Oxo-L-Norleucine (Don) in human neoplastic disease. Cancer. 1957;10(6):1138–50.
Alt J, Potter MC, Rojas C, Slusher BS. Bioanalysis of 6-diazo-5-oxo-l-norleucine in plasma and brain by ultra-performance liquid chromatography mass spectrometry. Anal Biochem. 2015;474:28–34.
Mueller C, Al-Batran S, Jaeger E, Schmidt B, Bausch M, Unger C, Sethuraman N: A phase IIa study of PEGylated glutaminase (PEG-PGA) plus 6-diazo-5-oxo-L-norleucine (DON) in patients with advanced refractory solid tumors. Journal of Clinical Oncology 2008, 26(15_suppl):2533–2533.
Hanaford AR, Alt J, Rais R, Wang SZ, Kaur H, Thorek DLJ, Eberhart CG, Slusher BS, Martin AM, Raabe EH. Orally bioavailable glutamine antagonist prodrug JHU-083 penetrates mouse brain and suppresses the growth of MYC-driven medulloblastoma. Translational oncology. 2019;12(10):1314–22.
Ahluwalia GS, Grem JL, Hao Z, Cooney DA. Metabolism and action of amino acid analog anti-cancer agents. Pharmacol Ther. 1990;46(2):243–71.
Sullivan MP, Nelson JA, Feldman S, Van Nguyen B. Pharmacokinetic and phase I study of intravenous DON (6-diazo-5-oxo-L-norleucine) in children. Cancer Chemother Pharmacol. 1988;21:78–84.
Pillai R, LeBoeuf SE, Hao Y, New C, Blum JLE, Rashidfarrokhi A, Huang SM, Bahamon C, Wu WL, Karadal-Ferrena B et al: Glutamine antagonist DRP-104 suppresses tumor growth and enhances response to checkpoint blockade in KEAP1 mutant lung cancer. Sci Adv 2024, 10(13):eadm9859.
Yokoyama Y, Estok TM, Wild R. Sirpiglenastat (DRP-104) induces antitumor efficacy through direct, broad antagonism of glutamine metabolism and stimulation of the innate and adaptive immune systems. Mol Cancer Ther. 2022;21(10):1561–72.
Iannitti T, Palmieri B. Clinical and experimental applications of sodium phenylbutyrate. Drugs R D. 2011;11(3):227–49.
Heo YA. Sodium Phenylbutyrate and Ursodoxicoltaurine: First Approval. CNS Drugs. 2022;36(9):1007–13.
Palir N, Ruiter JPN, Wanders RJA, Houtkooper RH. Identification of enzymes involved in oxidation of phenylbutyrate. J Lipid Res. 2017;58(5):955–61.
Kusaczuk M, Kretowski R, Bartoszewicz M, Cechowska-Pasko M. Phenylbutyrate-a pan-HDAC inhibitor-suppresses proliferation of glioblastoma LN-229 cell line. Tumour Biol. 2016;37(1):931–42.
Phuphanich S, Baker SD, Grossman SA, Carson KA, Gilbert MR, Fisher JD, Carducci MA. Oral sodium phenylbutyrate in patients with recurrent malignant gliomas: a dose escalation and pharmacologic study. Neuro Oncol. 2005;7(2):177–82.
Darmaun D, Welch S, Rini A, Sager BK, Altomare A, Haymond MW. Phenylbutyrate-induced glutamine depletion in humans: effect on leucine metabolism. Am J Physiol. 1998;274(5):E801–807.
Gilbert J, Baker SD, Bowling MK, Grochow L, Figg WD, Zabelina Y, Donehower RC, Carducci MA. A phase I dose escalation and bioavailability study of oral sodium phenylbutyrate in patients with refractory solid tumor malignancies. Clin Cancer Res. 2001;7(8):2292–300.
Mueller C, Al-Batran S, Jaeger E, Schmidt B, Bausch M, Unger C, Sethuraman N: A phase IIa study of PEGylated glutaminase (PEG-PGA) plus 6-diazo-5-oxo-L-norleucine (DON) in patients with advanced refractory solid tumors. In: ASCO. vol. 26: J Clin Oncol 2008.
Owen OE, Smalley KJ, D’Alessio DA, Mozzoli MA, Dawson EK. Protein, fat, and carbohydrate requirements during starvation: anaplerosis and cataplerosis. Am J Clin Nutr. 1998;68(1):12–34.
Emadi A, Zokaee H, Sausville EA. Asparaginase in the treatment of non-ALL hematologic malignancies. Cancer Chemother Pharmacol. 2014;73(5):875–83.
Chan WK, Horvath TD, Tan L, Link T, Harutyunyan KG, Pontikos MA, Anishkin A, Du D, Martin LA, Yin E, et al. Glutaminase Activity of L-Asparaginase Contributes to Durable Preclinical Activity against Acute Lymphoblastic Leukemia. Mol Cancer Ther. 2019;18(9):1587–92.
Sankaran H, Sengupta S, Purohit V, Kotagere A, Moulik NR, Prasad M, Dhamne C, Narula G, Banavali S, Gota V: A comparison of asparaginase activity in generic formulations of E.coli derived L- asparaginase: In-vitro study and retrospective analysis of asparaginase monitoring in pediatric patients with leukemia. Br J Clin Pharmacol 2020, 86(6):1081–1088.
P Hammel I El-Hariry T Macarulla R Garcia-Carbonero J-P Metges O Bouché F Portales RA Pazo Cid L Mineur AM Cubillo Gracian 2022 Trybeca-1: A randomized, phase 3 study of eryaspase in combination with chemotherapy versus chemotherapy alone as second-line treatment in patients with advanced pancreatic adenocarcinoma (NCT03665441) American Society of Clinical Oncology In.
Ohba S, Hirose Y. L-asparaginase and 6-diazo-5-oxo-L-norleucine synergistically inhibit the growth of glioblastoma cells. J Neurooncol. 2020;146(3):469–75.
Van Trimpont M, Peeters E, De Visser Y, Schalk AM, Mondelaers V, De Moerloose B, Lavie A, Lammens T, Goossens S, Van Vlierberghe P. Novel insights on the use of L-asparaginase as an efficient and safe anti-cancer therapy. Cancers (Basel). 2022;14(4):902.
Recouvreux MV, Grenier SF, Zhang Y, Esparza E, Lambies G, Galapate CM, Maganti S, Duong-Polk K, Bhullar D, Naeem R, et al. Glutamine mimicry suppresses tumor progression through asparagine metabolism in pancreatic ductal adenocarcinoma. Nat Cancer. 2024;5(1):100–13.
Yamashita AS, da Costa Rosa M, Stumpo V, Rais R, Slusher BS, Riggins GJ. The glutamine antagonist prodrug JHU-083 slows malignant glioma growth and disrupts mTOR signaling. Neurooncol Adv. 2021;3(1):vdaa149.
Harding JJ, Telli M, Munster P, Voss MH, Infante JR, DeMichele A, Dunphy M, Le MH, Molineaux C, Orford K, et al. A Phase I Dose-Escalation and Expansion Study of Telaglenastat in Patients with Advanced or Metastatic Solid Tumors. Clin Cancer Res. 2021;27(18):4994–5003.
Gross MI, Demo SD, Dennison JB, Chen L, Chernov-Rogan T, Goyal B, Janes JR, Laidig GJ, Lewis ER, Li J. Antitumor Activity of the Glutaminase Inhibitor CB-839 in Triple-Negative Breast CancerAntitumor Activity of the Glutaminase Inhibitor CB-839 in TNBC. Mol Cancer Ther. 2014;13(4):890–901.
Katt WP, Cerione RA. Glutaminase regulation in cancer cells: a druggable chain of events. Drug Discovery Today. 2014;19(4):450–7.
Schulte ML, Fu A, Zhao P, Li J, Geng L, Smith ST, Kondo J, Coffey RJ, Johnson MO, Rathmell JC, et al. Pharmacological blockade of ASCT2-dependent glutamine transport leads to antitumor efficacy in preclinical models. Nat Med. 2018;24(2):194–202.
Hidalgo M, Rodriguez G, Kuhn JG, Brown T, Weiss G, MacGovren JP, Von Hoff DD, Rowinsky EK. A Phase I and pharmacological study of the glutamine antagonist acivicin with the amino acid solution aminosyn in patients with advanced solid malignancies. Clin Cancer Res. 1998;4(11):2763–70.
Sun Y, Feng X, Liu X, Qian C, Che X, Cao F, Jin S, Meng D. Caudatan A, an undescribed human kidney-type glutaminase inhibitor with tetracyclic flavan from Ohwia caudata. Phytochemistry. 2018;152:22–8.
Wu C, Zheng M, Gao S, Luan S, Cheng L, Wang L, Li J, Chen L, Li H. A natural inhibitor of kidney-type glutaminase: a withanolide from Physalis pubescens with potent anti-tumor activity. Oncotarget. 2017;8(69):113516–30.
Sun W, Luan S, Qi C, Tong Q, Yan S, Li H, Zhang Y. Aspulvinone O, a natural inhibitor of GOT1 suppresses pancreatic ductal adenocarcinoma cells growth by interfering glutamine metabolism. Cell Commun Signal. 2019;17(1):111.
SH Kizilbash S McBrayer J Port JM Reid I Lanza JB Allred A Chakravarti C Kunos AA Adjei 2019 A phase Ib trial of CB-839 (telaglenastat) in combination with radiation therapy and temozolomide in patients with IDH-mutated diffuse astrocytoma and anaplastic astrocytoma (NCT03528642) American Society of Clinical Oncology In.
Konopleva M, DiNardo C, Bhagat T, Baran N, Lodi A, Saxena K, Cai T, Su X, Skwarska A, Guerra V et al: Glutaminase inhibition in combination with azacytidine in myelodysplastic syndromes: Clinical efficacy and correlative analyses. Res Sq 2023.
Tannir NM, Agarwal N, Porta C, Lawrence NJ, Motzer R, McGregor B, Lee RJ, Jain RK, Davis N, Appleman LJ, et al. Efficacy and Safety of Telaglenastat Plus Cabozantinib vs Placebo Plus Cabozantinib in Patients With Advanced Renal Cell Carcinoma: The CANTATA Randomized Clinical Trial. JAMA Oncol. 2022;8(10):1411–8.
Spigel DR, Akerley W, Evangelist M, Johnson M, Levy B, Owonikoko T, Paik P, Papagiannakopoulos T, Reckamp K, Akella L: P47. 07 KEAPSAKE Study of Telaglenastat vs Placebo Plus Standard-of-Care in 1L KEAP1/NRF2-Mutated Non-Squamous Metastatic NSCLC. Journal of Thoracic Oncology 2021, 16(10):S1099.
Philip PA, Bahary N, Mahipal A, Kasi A, Rocha Lima CMSP, Alistar AT, Oberstein PE, Golan T, Sahai V, Metges JP. Phase 3, multicenter, randomized study of CPI-613 with modified FOLFIRINOX (mFFX) versus FOLFIRINOX (FFX) as first-line therapy for patients with metastatic adenocarcinoma of the pancreas (AVENGER500). In.: American Society of Clinical Oncology; 2022.
Pardee TS, Lee K, Luddy J, Maturo C, Rodriguez R, Isom S, Miller LD, Stadelman KM, Levitan D, Hurd D. A Phase I Study of the First-in-Class Antimitochondrial Metabolism Agent, CPI-613, in Patients with Advanced Hematologic MalignanciesA Phase I Study of CPI-613. Clin Cancer Res. 2014;20(20):5255–64.
Alistar A, Morris BB, Desnoyer R, Klepin HD, Hosseinzadeh K, Clark C, Cameron A, Leyendecker J, D’Agostino R Jr, Topaloglu U, et al. Safety and tolerability of the first-in-class agent CPI-613 in combination with modified FOLFIRINOX in patients with metastatic pancreatic cancer: a single-centre, open-label, dose-escalation, phase 1 trial. Lancet Oncol. 2017;18(6):770–8.
Mukherjee P, Greenwood B, Henao J, Kiebish MA, Seyfried TN: Ketogenic diet as a metabolic vehicle for enhancing the therapeutic efficacy of mebendazole and devimistat in preclinical pediatric glioma. bioRxiv 2023:2023.2006. 2009.544252.
Jin L, Alesi GN, Kang S. Glutaminolysis as a target for cancer therapy. Oncogene. 2016;35(28):3619–25.
Lewerenz J, Albrecht P, Tien ML, Henke N, Karumbayaram S, Kornblum HI, Wiedau-Pazos M, Schubert D, Maher P, Methner A. Induction of Nrf2 and xCT are involved in the action of the neuroprotective antibiotic ceftriaxone in vitro. J Neurochem. 2009;111(2):332–43.
Rothstein JD, Patel S, Regan MR, Haenggeli C, Huang YH, Bergles DE, Jin L, Dykes Hoberg M, Vidensky S, Chung DS, et al. Beta-lactam antibiotics offer neuroprotection by increasing glutamate transporter expression. Nature. 2005;433(7021):73–7.
Li C, Allen A, Kwagh J, Doliba NM, Qin W, Najafi H, Collins HW, Matschinsky FM, Stanley CA, Smith TJ. Green tea polyphenols modulate insulin secretion by inhibiting glutamate dehydrogenase. J Biol Chem. 2006;281(15):10214–21.
Carmo F, Silva C, Martel F. Inhibition of Glutamine Cellular Uptake Contributes to the Cytotoxic Effect of Xanthohumol in Triple-Negative Breast Cancer Cells. Nutr Cancer. 2022;74(9):3413–30.
Lodi A, Saha A, Lu X, Wang B, Sentandreu E, Collins M, Kolonin MG, DiGiovanni J, Tiziani S. Combinatorial treatment with natural compounds in prostate cancer inhibits prostate tumor growth and leads to key modulations of cancer cell metabolism. NPJ precision oncology. 2017;1(1):1–12.
Tabrez S, Zughaibi TA, Hoque M, Suhail M, Khan MI, Khan AU. Targeting Glutaminase by Natural Compounds: Structure-Based Virtual Screening and Molecular Dynamics Simulation Approach to Suppress Cancer Progression. Molecules. 2022;27(15):5042.
Tyszka-Czochara M, Bukowska-Strakova K, Kocemba-Pilarczyk KA, Majka M. Caffeic acid targets AMPK signaling and regulates tricarboxylic acid cycle anaplerosis while metformin downregulates HIF-1α-induced glycolytic enzymes in human cervical squamous cell carcinoma lines. Nutrients. 2018;10(7):841.
Fan W-h, Wang F-c. Jin Z, Zhu L, Zhang J-x: Curcumin Synergizes with Cisplatin to Inhibit Colon Cancer through Targeting the MicroRNA-137-Glutaminase Axis. Current Medical Science. 2022;42(1):108–17.
Lee YM, Lee G, Oh TI, Kim BM, Shim DW, Lee KH, Kim YJ, Lim BO, Lim JH. Inhibition of glutamine utilization sensitizes lung cancer cells to apigenin-induced apoptosis resulting from metabolic and oxidative stress. Int J Oncol. 2016;48(1):399–408.
Zhang P, Wang Q, Lin Z, Yang P, Dou K, Zhang R. Berberine Inhibits Growth of Liver Cancer Cells by Suppressing Glutamine Uptake. Onco Targets Ther. 2019;12:11751–63.
Cerella C, Radogna F, Dicato M, Diederich M: Natural compounds as regulators of the cancer cell metabolism. Int J Cell Biol 2013, 2013.
Colwell N, Larion M, Giles AJ, Seldomridge AN, Sizdahkhani S, Gilbert MR, Park DM. Hypoxia in the glioblastoma microenvironment: shaping the phenotype of cancer stem-like cells. Neuro Oncol. 2017;19(7):887–96.
Olivier C, Oliver L, Lalier L, Vallette FM. Drug Resistance in Glioblastoma: The Two Faces of Oxidative Stress. Front Mol Biosci. 2020;7: 620677.
Pombo Antunes AR, Scheyltjens I, Duerinck J, Neyns B, Movahedi K, Van Ginderachter JA: Understanding the glioblastoma immune microenvironment as basis for the development of new immunotherapeutic strategies. Elife 2020, 9.
Al-Kharboosh R, ReFaey K, Lara-Velazquez M, Grewal SS, Imitola J, Quinones-Hinojosa A. Inflammatory Mediators in Glioma Microenvironment Play a Dual Role in Gliomagenesis and Mesenchymal Stem Cell Homing: Implication for Cellular Therapy. Mayo Clin Proc Innov Qual Outcomes. 2020;4(4):443–59.
Mosteiro A, Pedrosa L, Ferres A, Diao D, Sierra A, Gonzalez JJ. The Vascular Microenvironment in Glioblastoma: A Comprehensive Review. Biomedicines. 2022;10(6):1285.
Jandrey EHF, Bezerra M, Inoue LT, Furnari FB, Camargo AA, Costa ET. A Key Pathway to Cancer Resilience: The Role of Autophagy in Glioblastomas. Front Oncol. 2021;11: 652133.
Uribe D, Niechi I, Rackov G, Erices JI, San Martin R, Quezada C. Adapt to Persist: Glioblastoma Microenvironment and Epigenetic Regulation on Cell Plasticity. Biology (Basel). 2022;11(2):313.
Fletcher-Sananikone E, Kanji S, Tomimatsu N, Di Cristofaro LFM, Kollipara RK, Saha D, Floyd JR, Sung P, Hromas R, Burns TC. Elimination of Radiation-Induced Senescence in the Brain Tumor Microenvironment Attenuates Glioblastoma RecurrenceRadiation-Induced Senescence as a Driver of GBM Recurrence. Can Res. 2021;81(23):5935–47.
Dono A, Nickles J, Rodriguez-Armendariz AG, McFarland BC, Ajami NJ, Ballester LY, Wargo JA, Esquenazi Y. Glioma and the gut–brain axis: opportunities and future perspectives. Neuro-Oncology Advances. 2022;4(1):vdac054.
Hausmann D, Hoffmann DC, Venkataramani V, Jung E, Horschitz S, Tetzlaff SK, Jabali A, Hai L, Kessler T, Azorin DD, et al. Autonomous rhythmic activity in glioma networks drives brain tumour growth. Nature. 2023;613(7942):179–86.
Yang T, Liu D, Fang S, Ma W, Wang Y. Cytomegalovirus and Glioblastoma: A Review of the Biological Associations and Therapeutic Strategies. J Clin Med. 2022;11(17):5221.
Peredo-Harvey I, Rahbar A, Söderberg-Nauclér C. Presence of the human cytomegalovirus in glioblastomas—A systematic review. Cancers (Basel). 2021;13(20):5051.
Hochhalter CB, Carr C, O’Neill BE, Ware ML, Strong MJ. The association between human cytomegalovirus and glioblastomas: a review. Neuroimmunology Neuroinflammation. 2017;4:96–108.
Merlo LM, Pepper JW, Reid BJ, Maley CC. Cancer as an evolutionary and ecological process. Nat Rev Cancer. 2006;6(12):924–35.
Kroemer G, McQuade JL, Merad M, Andre F, Zitvogel L. Bodywide ecological interventions on cancer. Nat Med. 2023;29(1):59–74.
Tamiz AP, Koroshetz WJ, Dhruv NT, Jett DA. A focus on the neural exposome. Neuron. 2022;110(8):1286–9.
Hopkins BD, Goncalves MD, Cantley LC. Obesity and Cancer Mechanisms: Cancer Metabolism. J Clin Oncol. 2016;34(35):4277–83.
Srinivasan M, Arzoun H, Gk LB, Thangaraj SR: A Systematic Review: Does Insulin Resistance Affect the Risk and Survival Outcome of Breast Cancer in Women? Cureus 2022, 14(1).
Goncalves MD, Farooki A. Management of Phosphatidylinositol-3-Kinase Inhibitor-Associated Hyperglycemia. Integr Cancer Ther. 2022;21:15347354211073164.
Bernstock JD, Blitz SE, Hoffman SE, Gerstl JVE, Chiocca EA, Friedman GK. Recent oncolytic virotherapy clinical trials outline a roadmap for the treatment of high-grade glioma. Neurooncol Adv. 2023;5(1):vdad081.
Sestito S, Runfola M, Tonelli M, Chiellini G, Rapposelli S. New Multitarget Approaches in the War Against Glioblastoma: A Mini-Perspective. Front Pharmacol. 2018;9:874.
Yang L, TeSlaa T, Ng S, Nofal M, Wang L, Lan T, Zeng X, Cowan A, McBride M, Lu W, et al. Ketogenic diet and chemotherapy combine to disrupt pancreatic cancer metabolism and growth. Med. 2022;3(2):119–36.
Jia Q, Wang A, Yuan Y, Zhu B, Long H. Heterogeneity of the tumor immune microenvironment and its clinical relevance. Exp Hematol Oncol. 2022;11(1):24.
Lee AH, Sun L, Mochizuki AY, Reynoso JG, Orpilla J, Chow F, Kienzler JC, Everson RG, Nathanson DA, Bensinger SJ, et al. Neoadjuvant PD-1 blockade induces T cell and cDC1 activation but fails to overcome the immunosuppressive tumor associated macrophages in recurrent glioblastoma. Nat Commun. 2021;12(1):6938.
Arrieta VA, Dmello C, McGrail DJ, Brat DJ, Lee-Chang C, Heimberger AB, Chand D, Stupp R, Sonabend AM: Immune checkpoint blockade in glioblastoma: from tumor heterogeneity to personalized treatment. J Clin Invest 2023, 133(2).
Latzer P, Zelba H, Battke F, Reinhardt A, Shao B, Bartsch O, Rabsteyn A, Harter J, Schulze M, Okech T, et al. A real-world observation of patients with glioblastoma treated with a personalized peptide vaccine. Nat Commun. 2024;15(1):6870.
Hu JL, Omofoye OA, Rudnick JD, Kim S, Tighiouart M, Phuphanich S, Wang H, Mazer M, Ganaway T, Chu RM, et al. A Phase I Study of Autologous Dendritic Cell Vaccine Pulsed with Allogeneic Stem-like Cell Line Lysate in Patients with Newly Diagnosed or Recurrent Glioblastoma. Clin Cancer Res. 2022;28(4):689–96.
Sims D, Liman AK, Leung V, Hwang A, Means J, Liman AD. What We Have Learned About Combining a Ketogenic Diet and Chemoimmunotherapy: a Case Report and Review of Literature. Fed Pract. 2023;40(Suppl 3):S98.
Leone RD, Zhao L, Englert JM, Sun IM, Oh MH, Sun IH, Arwood ML, Bettencourt IA, Patel CH, Wen J, et al. Glutamine blockade induces divergent metabolic programs to overcome tumor immune evasion. Science. 2019;366(6468):1013–21.
Murphy S, Rahmy S, Gan D, Zhu Y, Manyak M, Li J, Lu X, Lu X: Overcome Prostate Cancer Resistance to Immune Checkpoint Therapy with Ketogenic Diet-Induced Epigenetic Reprogramming. bioRxiv 2023:2023.2008. 2007.552383.
Dai X, Bu X, Gao Y, Guo J, Hu J, Jiang C, Zhang Z, Xu K, Duan J, He S, et al. Energy status dictates PD-L1 protein abundance and anti-tumor immunity to enable checkpoint blockade. Mol Cell. 2021;81(11):2317–2331 e2316.
de Groot S, Lugtenberg RT, Cohen D, Welters MJ, Ehsan I, Vreeswijk MP, Smit VT, de Graaf H, Heijns JB, Portielje JE. Fasting mimicking diet as an adjunct to neoadjuvant chemotherapy for breast cancer in the multicentre randomized phase 2 DIRECT trial. Nat Commun. 2020;11(1):3083.
Yang H, Zingaro VA, Lincoff J, Tom H, Oikawa S, Oses-Prieto JA, Edmondson Q, Seiple I, Shah H, Kajimura S, et al. Remodelling of the translatome controls diet and its impact on tumorigenesis. Nature. 2024;633(8028):189–97.
Fu L, Jin W, Zhang J, Zhu L, Lu J, Zhen Y, Zhang L, Ouyang L, Liu B, Yu H. Repurposing non-oncology small-molecule drugs to improve cancer therapy: Current situation and future directions. Acta Pharm Sin B. 2022;12(2):532–57.
Lyne SB, Yamini B. An Alternative Pipeline for Glioblastoma Therapeutics: A Systematic Review of Drug Repurposing in Glioblastoma. Cancers (Basel). 2021;13(8):1953.
Armando RG, Mengual Gomez DL, Gomez DE. New drugs are not enough-drug repositioning in oncology: An update. Int J Oncol. 2020;56(3):651–84.
Leighl NB, Nirmalakumar S, Ezeife DA, Gyawali B. An Arm and a Leg: The Rising Cost of Cancer Drugs and Impact on Access. Am Soc Clin Oncol Educ Book. 2021;41:1–12.
Furuta T, Sabit H, Dong Y, Miyashita K, Kinoshita M, Uchiyama N, Hayashi Y, Hayashi Y, Minamoto T, Nakada M. Biological basis and clinical study of glycogen synthase kinase- 3beta-targeted therapy by drug repositioning for glioblastoma. Oncotarget. 2017;8(14):22811–24.
Slavc I, Mayr L, Stepien N, Gojo J, Aliotti Lippolis M, Azizi AA, Chocholous M, Baumgartner A, Hedrich CS, Holm S, et al. Improved Long-Term Survival of Patients with Recurrent Medulloblastoma Treated with a “MEMMAT-like” Metronomic Antiangiogenic Approach. Cancers (Basel). 2022;14(20):5128.
Zapletalova D, Andre N, Deak L, Kyr M, Bajciova V, Mudry P, Dubska L, Demlova R, Pavelka Z, Zitterbart K, et al. Metronomic chemotherapy with the COMBAT regimen in advanced pediatric malignancies: a multicenter experience. Oncology. 2012;82(5):249–60.
Kast RE, Alfieri A, Assi HI, Burns TC, Elyamany AM, Gonzalez-Cao M, Karpel-Massler G, Marosi C, Salacz ME, Sardi I, et al. MDACT: A New Principle of Adjunctive Cancer Treatment Using Combinations of Multiple Repurposed Drugs, with an Example Regimen. Cancers (Basel). 2022;14(10):2563.
O’Rawe M, Wickremesekera AC, Pandey R, Young D, Sim D, FitzJohn T, Burgess C, Kaye AH, Tan ST. Treatment of glioblastoma with re-purposed renin-angiotensin system modulators: Results of a phase I clinical trial. J Clin Neurosci. 2022;95:48–54.
Kwt K. Cho WCS: Drug Repurposing for Cancer Therapy in the Era of Precision Medicine. Curr Mol Pharmacol. 2022;15(7):895–903.
Maley CC, Aktipis A, Graham TA, Sottoriva A, Boddy AM, Janiszewska M, Silva AS, Gerlinger M, Yuan Y, Pienta KJ, et al. Classifying the evolutionary and ecological features of neoplasms. Nat Rev Cancer. 2017;17(10):605–19.
Bonavida B, Bharti AC, Aggarwal BB: Role of nutraceuticals in cancer chemosensitization: Academic Press; 2017.
Calvaruso M, Pucci G, Musso R, Bravata V, Cammarata FP, Russo G, Forte GI, Minafra L. Nutraceutical Compounds as Sensitizers for Cancer Treatment in Radiation Therapy. Int J Mol Sci. 2019;20(21):5267.
Chu M, Zheng C, Chen C, Song G, Hu X, Wang Z-w: Targeting cancer stem cells by nutraceuticals for cancer therapy. In: Seminars in Cancer Biology: 2021: Elsevier; 2021.
De Pergola G, Marucci S, Corbo F, Almerighi G, Cerutti N, Triggiani V, De Vito D, Castellana F, Zupo R: Nutraceuticals and Oral Supplements in Cancer Prevention: A Narrative Review. Endocrine, Metabolic Immune Disorders Drug Targets 2022.
Maiuolo J, Gliozzi M, Carresi C, Musolino V, Oppedisano F, Scarano F, Nucera S, Scicchitano M, Bosco F, Macri R, et al. Nutraceuticals and Cancer: Potential for Natural Polyphenols. Nutrients. 2021;13(11):3834.
Shukla Y, George J. Combinatorial strategies employing nutraceuticals for cancer development. Ann N Y Acad Sci. 2011;1229(1):162–75.
Ng JY, Munford V, Thakar H. Web-based online resources about adverse interactions or side effects associated with complementary and alternative medicine: a systematic review, summarization and quality assessment. BMC Med Inform Decis Mak. 2020;20(1):290.
Ambrosone CB, Zirpoli GR, Hutson AD, McCann WE, McCann SE, Barlow WE, Kelly KM, Cannioto R, Sucheston-Campbell LE, Hershman DL, et al. Dietary Supplement Use During Chemotherapy and Survival Outcomes of Patients With Breast Cancer Enrolled in a Cooperative Group Clinical Trial (SWOG S0221). J Clin Oncol. 2020;38(8):804–14.
Calvani M, Pasha A, Favre C. Nutraceutical Boom in Cancer: Inside the Labyrinth of Reactive Oxygen Species. Int J Mol Sci. 2020;21(6):1936.
Jermini M, Dubois J, Rodondi PY, Zaman K, Buclin T, Csajka C, Orcurto A. L ER: Complementary medicine use during cancer treatment and potential herb-drug interactions from a cross-sectional study in an academic centre. Sci Rep. 2019;9(1):5078.
Segal R, Zwaal C, Green E, Tomasone JR, Loblaw A, Petrella T. Exercise for People with Cancer Guideline Development G: Exercise for people with cancer: a systematic review. Curr Oncol. 2017;24(4):e290–315.
Champ CE, Carpenter DJ, Diaz AK, Rosenberg J, Ackerson BG, Hyde PN. Resistance Training for Patients with Cancer: A Conceptual Framework for Maximizing Strength, Power, Functional Mobility, and Body Composition to Optimize Health and Outcomes. Sports Med. 2023;53(1):75–89.
Hofmann P. Cancer and Exercise: Warburg Hypothesis, Tumour Metabolism and High-Intensity Anaerobic Exercise. Sports (Basel). 2018;6(1):10.
Paulusma CC, Lamers WH, Broer S, van de Graaf SFJ. Amino acid metabolism, transport and signalling in the liver revisited. Biochem Pharmacol. 2022;201: 115074.
Cooper ID, Brookler KH, Crofts CAP. Rethinking Fragility Fractures in Type 2 Diabetes: The Link between Hyperinsulinaemia and Osteofragilitas. Biomedicines. 2021;9(9):1165.
Morishita S, Hamaue Y, Fukushima T, Tanaka T, Fu JB, Nakano J. Effect of Exercise on Mortality and Recurrence in Patients With Cancer: A Systematic Review and Meta-Analysis. Integr Cancer Ther. 2020;19:1534735420917462.
Cannioto RA, Hutson A, Dighe S, McCann W, McCann SE, Zirpoli GR, Barlow W, Kelly KM, DeNysschen CA, Hershman DL, et al. Physical Activity Before, During, and After Chemotherapy for High-Risk Breast Cancer: Relationships With Survival. J Natl Cancer Inst. 2021;113(1):54–63.
Ekblom-Bak E, Bojsen-Moller E, Wallin P, Paulsson S, Lindwall M, Rundqvist H, Bolam KA. Association Between Cardiorespiratory Fitness and Cancer Incidence and Cancer-Specific Mortality of Colon, Lung, and Prostate Cancer Among Swedish Men. JAMA Netw Open. 2023;6(6): e2321102.
Li R, Xia J, Zhang XI, Gathirua-Mwangi WG, Guo J, Li Y, McKenzie S, Song Y. Associations of Muscle Mass and Strength with All-Cause Mortality among US Older Adults. Med Sci Sports Exerc. 2018;50(3):458–67.
Campbell KL, Winters-Stone KM, Wiskemann J, May AM, Schwartz AL, Courneya KS, Zucker DS, Matthews CE, Ligibel JA, Gerber LH, et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med Sci Sports Exerc. 2019;51(11):2375–90.
Sandler CX, Matsuyama M, Jones TL, Bashford J, Langbecker D, Hayes SC. Physical activity and exercise in adults diagnosed with primary brain cancer: a systematic review. J Neurooncol. 2021;153(1):1–14.
McTiernan A, Friedenreich CM, Katzmarzyk PT, Powell KE, Macko R, Buchner D, Pescatello LS, Bloodgood B, Tennant B, Vaux-Bjerke A, et al. Physical Activity in Cancer Prevention and Survival: A Systematic Review. Med Sci Sports Exerc. 2019;51(6):1252–61.
Cook SA, Salmon P, Hayes G, Byrne A, Fisher PL. Predictors of emotional distress a year or more after diagnosis of cancer: A systematic review of the literature. Psychooncology. 2018;27(3):791–801.
Hulbert-Williams NJ, Beatty L, Dhillon HM. Psychological support for patients with cancer: evidence review and suggestions for future directions. Curr Opin Support Palliat Care. 2018;12(3):276–92.
Tan TT, Tan MP, Lam CL, Loh EC, Capelle DP, Zainuddin SI, Ang BT, Lim MA, Lai NZ, Tung YZ, et al. Mindful gratitude journaling: psychological distress, quality of life and suffering in advanced cancer: a randomised controlled trial. BMJ Support Palliat Care. 2023;13(e2):e389–96.
Nevin JT, Moussa M, Corwin WL, Mandoiu II, Srivastava PK. Sympathetic nervous tone limits the development of myeloid-derived suppressor cells. Sci Immunol. 2020;5(51):eaay9368.
Zhao H, Wu L, Yan G, Chen Y, Zhou M, Wu Y, Li Y. Inflammation and tumor progression: signaling pathways and targeted intervention. Signal Transduct Target Ther. 2021;6(1):263.
Shimba A, Ikuta K: Control of immunity by glucocorticoids in health and disease. In: Seminars in Immunopathology: 2020: Springer; 2020: 669–680.
Thompson G, Lawrie TA, Kernohan A, Jenkinson MD. Interval brain imaging for adults with cerebral glioma. Cochrane Database Syst Rev. 2019;12(12):CD013137.
Reiter MJ, Costello JE, Schwope RB, Lisanti CJ, Osswald MB. Review of Commonly Used Serum Tumor Markers and Their Relevance for Image Interpretation. J Comput Assist Tomogr. 2015;39(6):825–34.
Soda N, Clack K, Shiddiky MJA. Recent advances in liquid biopsy technologies for cancer biomarker detection. Sensors & Diagnostics. 2022;1(3):343–75.
Cohen JD, Li L, Wang Y, Thoburn C, Afsari B, Danilova L, Douville C, Javed AA, Wong F, Mattox A, et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science. 2018;359(6378):926–30.
Lu VM, Goyal A, Graffeo CS, Perry A, Burns TC, Parney IF, Quinones-Hinojosa A, Chaichana KL. Survival Benefit of Maximal Resection for Glioblastoma Reoperation in the Temozolomide Era: A Meta-Analysis. World Neurosurg. 2019;127:31–7.
Goenka A, Tiek D, Song X, Huang T, Hu B, Cheng SY. The Many Facets of Therapy Resistance and Tumor Recurrence in Glioblastoma. Cells. 2021;10(3):484.
Osuka S, Van Meir EG. Overcoming therapeutic resistance in glioblastoma: the way forward. J Clin Invest. 2017;127(2):415–26.
McBain C, Lawrie TA, Rogozinska E, Kernohan A, Robinson T, Jefferies S. Treatment options for progression or recurrence of glioblastoma: a network meta-analysis. Cochrane Database Syst Rev. 2021;5(1):CD013579.
Keating NL, Landrum MB, Rogers SO Jr, Baum SK, Virnig BA, Huskamp HA, Earle CC, Kahn KL. Physician factors associated with discussions about end-of-life care. Cancer. 2010;116(4):998–1006.
Daugherty CK, Hlubocky FJ. What are terminally ill cancer patients told about their expected deaths? A study of cancer physicians’ self-reports of prognosis disclosure. J Clin Oncol. 2008;26(36):5988.
Richardson TE, Kumar A, Xing C, Hatanpaa KJ, Walker JM. Overcoming the Odds: Toward a Molecular Profile of Long-Term Survival in Glioblastoma. J Neuropathol Exp Neurol. 2020;79(10):1031–7.
Brenner H. Long-term survival rates of cancer patients achieved by the end of the 20th century: a period analysis. Lancet. 2002;360(9340):1131–5.
Caplan AL, Ray A. The Ethical Challenges of Compassionate Use. JAMA. 2016;315(10):979–80.
Ahn E, Shin DW, Choi JY, Kang J, Kim DK, Kim H, Lee E, Hwang KO, Oh B, Cho B. The impact of awareness of terminal illness on quality of death and care decision making: a prospective nationwide survey of bereaved family members of advanced cancer patients. Psychooncology. 2013;22(12):2771–8.
Johnson SB, Butow PN, Kerridge I, Tattersall MHN. Patient autonomy and advance care planning: a qualitative study of oncologist and palliative care physicians’ perspectives. Support Care Cancer. 2018;26(2):565–74.
Carmona-Bayonas A, Rodriguez-Gonzalez A, García-García T, Velasco-Durantez V, Hernández-San Gil R, Cruz-Castellanos P, Fernandez-Montes A, Castillo-Trujillo A, Ballester I, Rogado J: Can Oncologists Prompt Patient Prognostic Awareness to Enhance Decision-Making? Data From the Neoetic Study. Oncologist 2023:oyad100.
DeBerardinis RJ, Chandel NS. We need to talk about the Warburg effect. Nat Metab. 2020;2(2):127–9.