Study design and participants
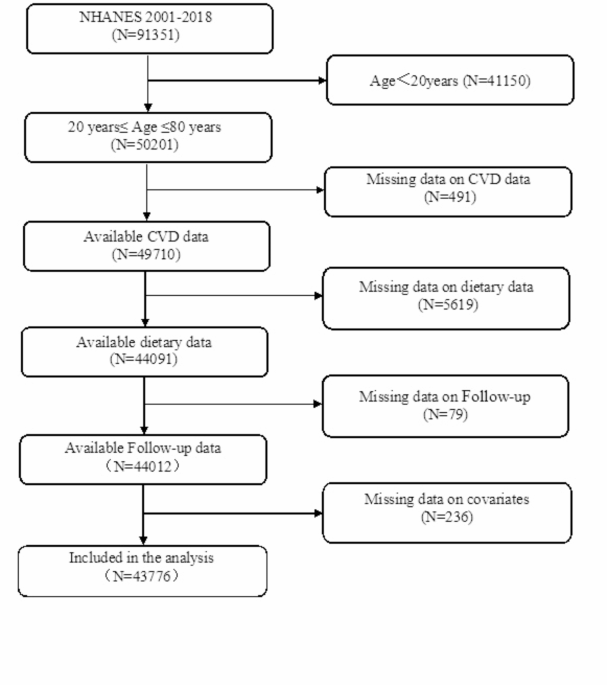
This cohort study utilized data from the nine national health and nutrition examination survey (NHANES) cycles conducted between 2001 and 2018, which included at least one dietary recall assessment (https://www.cdc.gov/nchs/NHANES/index). NHANES is a cross-sectional study initiated in 1999 by the National Center for Health Statistics (NCHS), aiming to evaluate the health and nutritional status of the non-institutional civilian population in the United States. To supplement this study, we linked the NHANES database from 2001 to 2018 with the NHANES Public Use Associated Mortality Archive, providing mortality follow-up data until December 31, 2019 (https://www.cdc.gov/nchs/data-linkage/ mortality.htm).The selection process of the study population is depicted in Fig. 1. A total of 91,351 participants were initially included in the retrospective cohort study. However, individuals below the age of 20 (N = 41,150), those with missing CVD data (N = 491), missing dietary data (N = 5619), missing follow-up data (N = 79), and those with missing covariate data (N = 236) were excluded from the analysis. Consequently, complete information on 43,776 adults was ultimately considered for the final analysis. All participants provided written informed consent, and the trial protocol of this study has been approved by the Ethics Review Committee at the National Center for Health Statistics.
Dietary intake data
Dietary intake data were collected through two 24-hour retrospective NHANES surveys conducted by trained dietary investigators. The initial survey was administered face-to-face, followed by a subsequent telephone survey within three to 10 days. In the follow-up survey, participants were requested to recall and report the types and quantities of various foods and beverages consumed in the preceding 24 h, with dietary intake estimated based on the average of these two recalls11. Energy and nutrient intakes for all food items were calculated using the Food and Nutrition database in dietary studies12.
The dietary ketogenic ratio(DKR)
To evaluate dietary patterns for achieving nutritional ketosis, we calculated the Dietary Ketogenic Ratio (DKR) based on the proportion of macronutrients in the diet with ketogenic and antiketogenic properties. The DKR for macronutrients was determined using the equation developed by Withrow13. Essentially, this calculation involves dividing (0.9×grams of fat + 0.46×grams of protein) by (0.1×grams of fat + 0.58 × grams of protein + grams of net carbohydrates), resulting in values ranging from 0 to 9. A higher DKR value indicates a greater likelihood of inducing nutritional ketosis.
Outcome variables
In this study, we evaluated all-cause mortality as the primary outcome measure, with secondary outcomes including mortality related to CVD. Information regarding vital status of participants was acquired from publicly accessible mortality data files. To establish a connection between death records in the National Death Index and continuous NHANES data, both probabilistic and deterministic approaches were employed by the National Center for Health Statistics. The success rate for establishing linkages surpassed 99%14. The observation period began at baseline (defined as the date of NHANES participation) and ended either upon occurrence of death or on December 31st, 2019.
Covariates
Information regarding sociodemographic and lifestyle characteristics was obtained from demographics and questionnaire data. This included information on age(Youth group,≤40 years; Middle-aged group, 40–60 years and Elderly group, ≥60 years), gender, Race/ethnicity (Mexican American、Non-Hispanic White、Non- Hispanic Black、Other Hispanic、Other Race), educational level(Less than High school、High school/GED, More than high school), family income to poverty ratio (PIR), marital status(Married, Widowed, Divorced, Separated, Never married, Living with partner), smoking status, and BMI (<18.5 kg/m2,18.5–24 kg/m2, 24–28 kg/m2, ≥28 kg/m2). Participants were categorized as smokers if they responded affirmatively to the query, “Have you smoked at least 100 cigarettes in your entire life?” Conversely, those who answered negatively were classified as non-smokers. Standing height (centimeter, cm) and weight (kilogram, kg) were measured at the mobile examination center. The Body Mass Index (BMI, kg/cm2) was calculated by dividing the weight by the square of standing height.
Participants were considered to have a history of cardiovascular disease if they had been diagnosed by a medical professional with congestive heart failure(CHF), coronary heart disease(CHD), angina/angina pectoris, and myocardial infarction(MI). The presence of hypertension, stroke, and cancer/malignancy was determined through questionnaire responses. The definition of hypertension encompassed self-reported hypertension, systolic blood pressure ≥ 140 mm Hg and/or diastolic blood pressure ≥ 90 mm Hg, or documented use of antihypertensive medication.Diabetes was defined as HbA1c ≥ 6.5% or self-reported use of glucose-lowering medications.
Multiple imputation techniques were employed to handle missing values in covariates, with the percentage of missing values being less than 10%. These covariates included PIR (missing 7.8%), BMI (missing 1.5%), hypertension (missing 0.2%), and no variables exhibited missing values exceeding 10%.
Statistical analysis
The participants were categorized into two groups based on their survival status.
The baseline characteristics were subjected to descriptive analysis, with continuous variables presented as mean ± standard deviation (SD) or median (interquartile range), while categorical variables were reported as counts and percentages.Between-group comparisons were conducted using appropriate statistical tests: the Student’s t-test for normally distributed continuous variables, the Wilcoxon rank-sum test for non-normally distributed variables, and the chi-square test for categorical variables.
The associations between DKR and all-cause and cardiovascular mortality were evaluated using multivariate Cox proportional hazard models, yielding hazard ratios (HRs) along with their corresponding 95% confidence intervals (CIs).The quartiles of DKR were utilized to calculate HRs, with Q1 serving as the reference group in Model A, which incorporated unadjusted covariates. Model B was adjusted for age, education level, race, marital status, and PIR. In Model C, additional covariates including BMI, diabetes mellitus, CHF, CHD, angina pectoris, MI, stroke history, and cancer diagnosis were included.
To investigate the dose-response relationship between DKR and all-cause and CVD mortality, we utilized multivariable adjusted restricted cubic splines (RCS) in model C to explore potential non-linear associations.
The statistical significance was determined at a two-tailed p-value of less than 0.05. All data were analyzed using SPSS 27 software. The data were generated by GraphPad Prism 9.4 and R version 3.6.