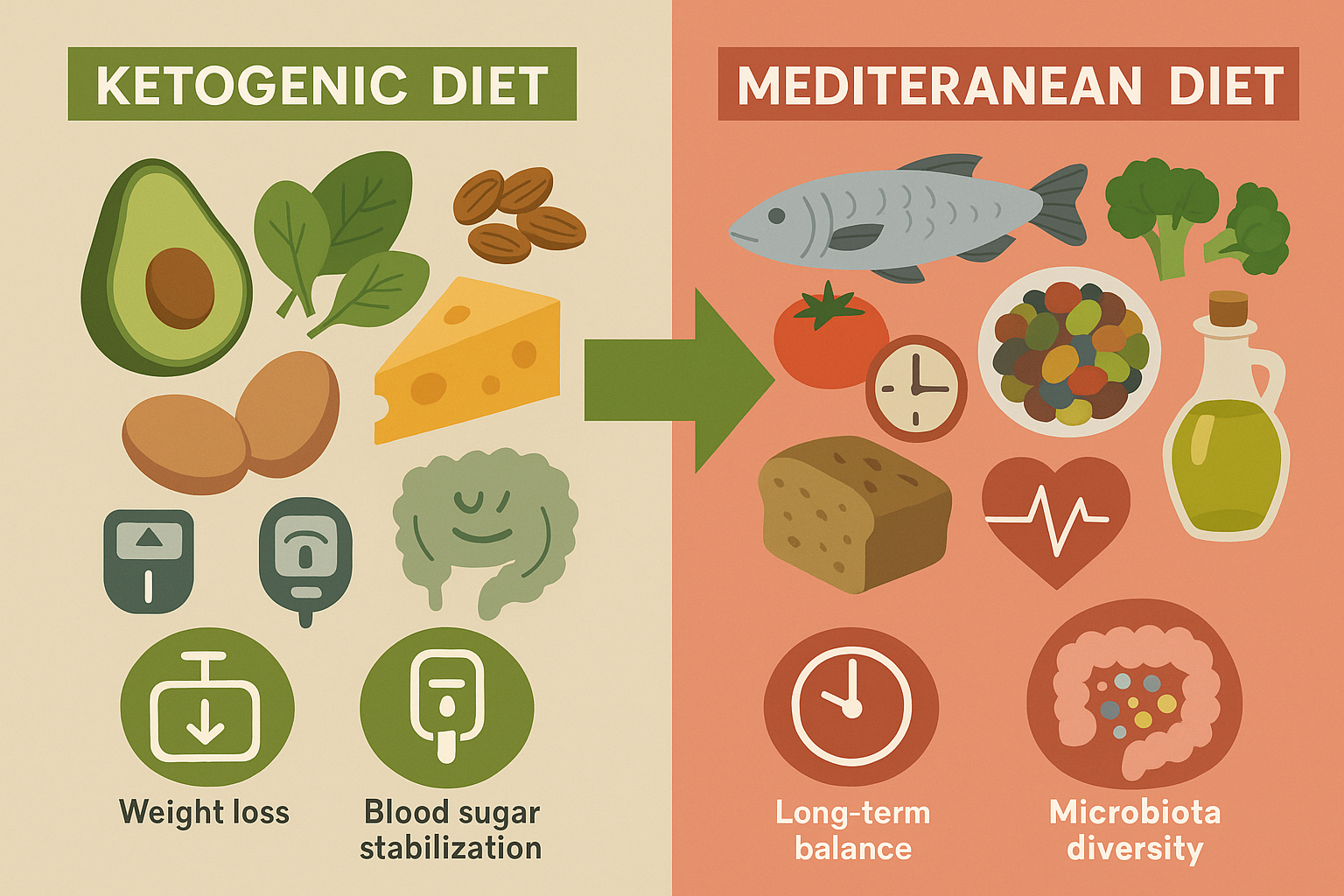
A 12-month pilot study published in Metabolites examined the effects of very-low-calorie ketogenic (VLCKD) and Mediterranean diets (MD) on gut microbiota and metabolic health in diabetic patients with newly diagnosed type 2 diabetes and obesity. Conducted in Brazil and Italy, the study followed 11 participants, with 8 completing the full duration. Initially, participants were randomized to either VLCKD or MD for the first three months, after which all transitioned to the Mediterranean diet.
Key Findings:
- Weight and Glycemic Control: By six months, the VLCKD group experienced significant reductions in BMI (−5.8 kg/m²) and HbA1c levels (−1.2%), indicating improved weight and blood sugar control. These improvements were more pronounced than those observed in the MD group.
- Gut Microbiota: VLCKD led to an increase in beneficial gut bacteria, notably Akkermansia, associated with enhanced gut barrier function and metabolic health. However, by the 12-month mark, the abundance of these beneficial microbes declined, suggesting that the positive effects on gut microbiota may diminish over time.
- Cholesterol Levels: An increase in LDL cholesterol was observed in the VLCKD group by the end of the study, raising potential concerns about long-term cardiovascular risks.
Interpretation of Results:
The results highlight that the very-low-calorie ketogenic diet (VLCKD) led to more dramatic improvements in several health metrics over the first six months compared to the Mediterranean diet (MD). Participants in the VLCKD group not only lost more weight and had sharper reductions in HbA1c (a marker of long-term blood sugar levels), but they also showed notable improvements in insulin sensitivity. This suggests that carbohydrate restriction may help stabilize blood glucose and reduce the need for medication in newly diagnosed type 2 diabetes patients.
Microbiota Shifts:
One particularly interesting aspect of the study was the shift in gut microbiota. Those on VLCKD showed an increase in Akkermansia muciniphila, a bacterial species linked to reduced inflammation and better metabolic outcomes. This bacterium has been associated with enhanced gut lining integrity, which can help lower systemic inflammation—a key contributor to insulin resistance and metabolic syndrome.
However, after the switch to the Mediterranean diet at month three, and particularly by month twelve, the abundance of these beneficial microbes declined. This suggests the microbiome improvements associated with VLCKD may be diet-dependent and not sustained without continued low-carb intake.
Cholesterol Concerns for Diabetic Patients:
One downside noted was the increase in LDL cholesterol in the VLCKD group by the end of the study. While weight loss and glycemic control improved, this rise in LDL could present a cardiovascular risk, especially for patients already predisposed to heart disease. The study did not report whether LDL particle size or HDL levels changed significantly, which could alter how this LDL increase should be interpreted.
Diet Transition Strategy:
All participants transitioned to the Mediterranean diet after three months, making this a hybrid intervention. The rationale was likely to combine the rapid metabolic improvements of VLCKD with the longer-term sustainability and cardiovascular benefits of the Mediterranean diet. This sequence may represent a more practical and safer long-term strategy for diabetic patients, though it may also dilute some of the microbiota-related benefits observed during the ketogenic phase.
The Conclusion for Diabetic Patients:
The study indicates that a very-low-calorie ketogenic diet (VLCKD) can offer superior short- to mid-term benefits in weight loss, glycemic control, and gut microbiota composition for patients with type 2 diabetes and obesity. These results are particularly relevant in the context of diabesity — a term used to describe the close link and frequent co-occurrence of diabetes and obesity, which together drive much of the global metabolic disease burden. The findings suggest that targeted dietary interventions, especially when personalized, can be powerful tools in managing this dual condition.
However, the sustainability of these benefits and potential long-term risks for diabetic patients — such as increased LDL cholesterol during VLCKD — require further investigation. The transition to a Mediterranean diet after the ketogenic phase appears to balance short-term gains with longer-term cardiovascular safety, offering a potentially effective phased approach to managing diabesity.
For more detailed information, you can access the full article here: Source link





